Pilot Evaluation of a Virtual Clinical Excursion (VCE) Among Senior Nursing Students: Part 2 Qualitative Perspectives and Learning Style
Loretta Secco, RN PhD
Donna Bulman, RN, PhD
Kathy Wilson, RN, PhD
Faculty of Nursing, University of New Brunswick
Funding Source
The research project was funded by a grant from Sigma Theta Tau International/National League of Nursing
Abstract
This brief describes the qualitative findings from a pilot study of a sample of seven, 4th year nursing students who completed a virtual clinical excursion (VCE) learning experience. The students completed a learning style inventory and an online survey to capture student perspectives on whether the VCE affected clinical judgement and preparedness for clinical practice. Students presented mixed reviews on the VCE learning experience. While some students reported improved confidence and preparedness for clinical practice, others noted scepticism due to lack of realism and interaction with patients and clinical instructors. Findings are discussed within the framework of learning styles and recommendations are offered for nurse educators.
Introduction
Due to the complexity of the health care system and high acuity of patient care, nurse educators are increasingly expected to prepare graduate nurses with clinical judgement and the requisite abilities to ensure safe nursing practice (Lasater, 2007). Teaching these clinical abilities is a major component of any education related to health care (Harder, 2010). To achieve this expectation many educators have integrated realistic simulation learning resources into their curriculum. In fact, one Canadian survey reported that 70% of nursing programs used simulations to augment clinical learning experience and 11% of these programs replaced from eight to forty hours of clinical practical hours with simulation experiences (Garrett, MacPhee, & Jackson, 2011). Many researchers have reported positive student responses to simulated patient manikins (Macy & Schrader, 2008; Yeager & Gotwals, 2010) and virtual clinical learning environments (Schmidt & Stewart, 2010) in various types of nursing practice (Yeager & Gotwals, 2010) and mock settings (Yeager & Gotwals, 2010). Positive findings include improved student outcomes related to clinical judgement such as confidence (Pike & O’Donnell, 2010), medication administration (Sears, Goldsworthy, & Goodman), critical thinking (Sulivan-Mann, Perron, & Fellner, 2009), and knowledge (Cant & Cooper, 2009).
While nurse educators are encouraged to integrate various simulation learning approaches, little is known about effectiveness for improved student learning or patient safety (Galloway, 2009). Four different student nurse viewpoints on simulation manikin learning have been identified: reflectors, reality sceptics, comfort seekers, and technology savvies, and learning style is also suggested as an important determinant of satisfaction with simulation learning (Baxter, Akhtar-Danesh, Valaitis, Stnyon, & Sproul, 2009). Greater knowledge about student nurses’ perspectives on simulated learning (Ford, Mazzone, & Taylor, 2005) would inform faculty about how these learning approaches fit within nursing programs. This study explored the learning styles and student perspectives of 4th year nursing students about whether a virtual clinical excursion (VCE) learning experience affected their clinical judgement and preparedness for senior clinical preceptorship.
Concepts and Methods
The study concepts included clinical judgment, preparedness for clinical practice, and learning style. Clinical judgment is defined as ‘… thinking and evaluative processes that focus on the nurse’s response to a patient’s ill-structured and multi-layered problems’ (Lasater, 2007) or the ‘ability to think like a nurse’(Cato, Lasater, & Peeples, 2009). Preparedness for clinical practice is defined as feeling ready and able to face challenges of a clinical learning rotation and provide competent nursing care. Learning style was measured with the 12-item Kolb Learning Styles Inventory (KLSI) (Kolb, 2007). The extent that students prefer four particular learning style dimensions are assessed: concrete experience (CE) or direct experience, feelings and emotions; reflective observations (RO) or looking back, remembering and gathering new information about an experience; abstract conceptualization (AC) or creating meaning from an experience as a guide for subsequent action, and active experimentation (AE) or testing a plan by carrying it out (Kayes, 2005).
Preference for two paired modes of learning, either CE versus AC for perceiving information or RO versus AE, for processing information defines individual ‘learning style’. When this information is plotted one of four particular learning styles is identified, i.e., diverging, assimilating, converging, or accommodating (Wang, Wang, Wang, & Huang, 2006). The diverging learner is imaginative, emotional and people-orientated while an assimilating learner is less interested in people, more interested in abstract concepts, and prefers basic over applied sciences. The converging learner finds uses for theories, likes to hypothesize and deal with things rather than people while the accommodating learner is highly action-orientated and relies more on information provided rather than their own analysis (Wang, et al., 2006).
All students in a 4th year course completed a KLSI and were oriented to the Evolve Elsevier medical surgical VCE (Mathers, 2007) in the classroom. After the orientation, 20 students who volunteered to use the VCE were given the print-based workbook and software DVD. After the students completed the senior clinical course, the study was approved by the University Ethics Board, and they had six weeks to provide opportunity to use the VCE, students were emailed a study explanation and invitation to complete the survey. The email contained a url to link those who volunteered to complete the online survey that contained three text boxes to collect information on student perspectives. The researchers emailed two additional reminder invitations and offered reimbursement honorarium ($15.00 money card) to improve student response rate.
Results
The final sample of seven, fourth year nursing students ranged from 21 to 37 years of age with an average age of 24.7 years. The nursing students included three (42.9%) diverging, two (28.6%) assimilating, and one each of converging and accommodating (14.2%) learning styles (Figure 1).
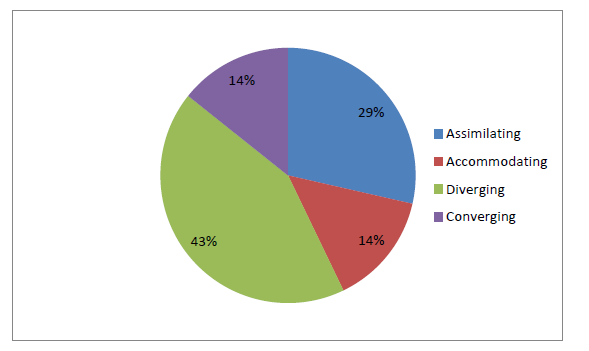
Figure 1. Learning Styles
Learning Styles and Qualitative Comments
One student with a diverging learning style commented that the VCE matched individual learning style and helped transfer knowledge to the clinical situation. ‘I really enjoyed using this tool in order to enhance learning. I do not just learn from reading out of a book, to use this VCE it gave me a practical experience, which helped me to remember things and transfer learning to my patient care.’ This comment appeared consistent with the diverging learner who combines concrete experience with reflective observation and prefers to observe rather than take action (Kolb, 2007) by providing a safe learning environment to “try out” different ways of approaching a novel situation. Another student with a diverging learning style reflected ‘… the program could be a little more user-friendly. However, I will say that as with anything the more I used it, it was easier to go through the simulations. It was a positive learning experience that I enjoyed.’
Some students who used the VCE made positive comments about the patient scenarios. For example, a student with an accommodating learning style noted that ‘it was cool to see the differing scenarios, some of which I hadn’t personally experienced in previous clinical settings’ and another diverging student commented that the VCE learning ‘… helped build confidence in nursing interventions and skills’. The same student described how the VCE improved stress levels as it ’… helped me remain calm during stressful situations because I felt as though I had “been through it before”. To some extent I know what to expect because of the VCE’. The same student noted that he/she ‘really enjoyed the chart – previous to VCE I really found charts extremely confusing and overwhelming.’
The one student with converging learning style commented on confidence:
‘I feel that this gave me confidence in my nursing interventions and skills because it made me realize that I am indeed competent with my nursing knowledge. I feel that I was knowledgeable about medications and ensuring I did not make any errors. I really enjoyed working through the scenarios… I would definitely recommend this program for other students.’
This positive evaluation is consistent with Kolb’s suggestion the converging learner has a preference for technical problems and experimentation with simulations and practical applications (Kolb, 2007). Consideration of one’s personal knowledge, skills and confidence with nursing interventions is consistent with reports of ‘reflectors’ as a major student viewpoint following simulation learning experiences (Baxter, et al., 2009). The same converging learning student noted improved clinical judgement and decision making:
‘I believe that it made my judgment better because it helped me to critically think through each scenario and to think about possible side effects and different outcomes to the patient’s health. I used the VCE during preceptorship during my days off. It made me confident in myself as a future new grad because it gave me some independence in making my own nursing decisions.’
One negative comment from a student with an assimilating learning style suggested skepticism and lack of realism: ‘But, over the last 4 years I believe I learned most on the floor and this learning tool is basic and not always the reality.’ Another assimilating student commented: ‘I don’t think I like it. Like I said it would be more beneficial earlier.’ These comments are consistent with the need for logical order required by most assimilating learners and their general dislike for role play type activities (Mackeracher, 1994). However, it is possible that an earlier introduction to the VCE may have been more positively evaluated. This skepticism is consistent with the widely held view that that simulation experiences will never replace ‘… real patients and the real world’ (Baxter, et al., 2009. pg. 861).
Three of the seven students in the current study suggested the VCE resource be placed in 2nd or 3rd year of the nursing program. ‘This tool should be introduced in 2nd year- although it helped me out lots in my fourth [year] it would have been a nice resource to have a few years ago!’ Another student noted: ‘I think this is a good tool to get students ready for clinical and perhaps throughout their clinical experience from year 1to 2. It gave me the basics to better prepare me for hospital clinical rotations.’ Another student stated ‘… I think it would be a great resource for students in 3rd year starting on medical surgical units. I already had developed most of the skills before trying the VCE.’ Another suggestion from a student was the need for more orientation and coaching: ‘I found the VCE and clinical learning application to be difficult to access and comprehend in the beginning. The instructions could be more clear or maybe the program could be a little more user-friendly.’
Discussion
The findings from this study are consistent with Baxter et al. (2009) who noted not all students enjoy simulation learning. The participants provided sage advice on the value of the VCE and best placement within the nursing curriculum. The suggestion by a student that the VCE be placed earlier in the nursing program is consistent with Schlairet and Pollock (2012) who noted junior nursing students were more satisfied with active learning, problem solving and self-confidence compared with senior students. The researchers reported that simulated clinical learning experience were as effective as traditional clinical experience with respect to knowledge acquisition (Schlairet & Pollock). Research is needed to establish whether there are any beneficial effects on student clinical performance or ability.
Students in this exploratory study reported various perspectives on whether the VCE prepared them for clinical practice in senior preceptorship. This variation may be related to differences in past clinical learning opportunities or learning style preference. Students who lacked clinical experience with the content of a particular VCE patient scenario may have rated learning resources more positively. In contrast, the student with previous experience with ‘real’ patients may suggest the VCE is more appropriate for novice student learners. The mixed review suggests VCEs may be appropriate learning resources for more junior students with less clinical experience. The student reports of increased confidence and lower stress suggested the VCE may best match learning needs of students who prefer greater preparation, rehearsal before clinical practice, or who have lower confidence.
The accommodating, diverging, and converging learning styles had more positive learning experiences compared with the assimilating students. The assimilating students reported greater skepticism and interest in ‘real’ experiences with actual patients and clinical instructors. This skeptics is similar to Seele et al. who noted surgery clerkship students preferred actual clinical experience, a clinical teacher, and the interpersonal element compared with a computer learning program (Steele, Johnson Palensky, Lynch, Lacy, & Duffy, 2002). Similarly, Feingold et al. noted less than fifty percent of nursing students in an advanced acute care course reported increased confidence and improved clinical competence after a simulated clinical learning experience with SimMan © ( 2004). Improved confidence and skill are two components of Lasater’s interactive model of clinical judgement development (Lasater, 2007) the exploratory findings suggest the VCE promoted student clinical judgement for a subset of students.
Several researchers have suggested that students who prefer simulation learning situations may have stronger critical thinking, problem solving abilities, and confidence (Vivien, Tham, Lau, Mei, & Kiat, 2010). Furthermore, 1st and 2nd year students have been evaluated as weak in critical thinking ability while also ‘curious to know how’ despite being ‘passive in seeking the truth’ (Vivien, et al., 2010). Research is needed to determine whether VCE learning opportunities with complex nursing care scenarios would promote independent learning, active participation, and critical thinking among junior students.
Recommendations
Limitations of this study include small sample size and lack of focus group sessions to assess whether the findings ring true for the student participants. Despite the limitations, several recommendations are offered for educators and researchers. It is recommended that nursing faculty consider student learning preferences, past clinical experience, and stage in the nursing program when planning VCE learning experiences. Such considerations would help match student preferences and learning needs with the particular VCE resource. Association of the VCE learning resource within a theory course might better situate student learning and create opportunity for the educator to encourage critical thinking and clinical judgment. Previous researchers noted that combined lecture and simulation teaching format with small groups of students effectively increased student satisfaction and consistency with learning style (Sinclair & Ferguson, 2009). Another recommendation is that nurse educators should not assume all nursing students enjoy virtual learning experiences. More rigorous research is recommended to determine whether this learning approach effectively lowers student anxiety or enhances feeling better prepared for clinical application with patients.
References
Baxter, P., Akhtar-Danesh, N., Valaitis, R., Stnyon, W., & Sproul, S. (2009). Simulated experiences: Nursing students share their perspectives. Nurse Education Today, 29, 859-866.
Cant, R. P., & Cooper, S. J. (2009). Simulated-based learning in nurse education: Systematic review. Journal of Advanced Nursing, 66(1), 3-15.
Cato, M. L., Lasater, K., & Peeples, A. I. (2009). Nursing students’ self-assessment of their simulation experiences. Nursing Education Perspectives, 30(2), 105.
Ford, G. S., Mazzone, M. A., & Taylor, K. (2005). Effect of computer-assisted instruction versus traditional modes of instruction on student learning of musculoskeletal special tests. Journal of Physical Therapy Education, 19(2), 22.
Galloway, S. (2009). Simulation techniques to bridge the gap between novice and competent healthcare professionals. The Online Journal of Issues in Nursing, 14(2), 3.
Garrett, B. M., MacPhee, M., & Jackson, C. (2011). Implementing high-fidelity simulation in Canada: Reflections on 3 years of practice. Nurse Education Today, 31(7), 671.
Harder, B. N. Use of simulation in teaching and learning in health sciences: a systematic review. Journal of Nursing Education, 49(1), 23.
Kayes, D. C. (2005). Internal validity and reliability of Kolb’s learning style inventory Version 3 (1999). Journal of Business and Psychology, 20(2), 249-257.
Kolb, D. A. (2007). Kolb Learning Style Inventory LSI Workbook v 3.1: Hay Group.
Lasater, K. (2007). High-fidelity simulation and the development of clinical judgment: Students’ experiences. Journal of Nursing Education, 46(6), 269-276. doi: DOI 1276789981
Macy, R., & Schrader, V. (2008). Pediophobia: A new challenge facing nursing faculty in clinical teaching by simulation. Clinical Simulation in Nursing, 4(3), e89.
Mathers, D. (2007). Virtual clinical excursion For Medial-Surgical Nursing, Pacific View Regional Hospital. St. Louis: Mosby/Elsevier.
Pike, T., & O’Donnell, V. (2010). The impact of clinical simulation on learner self-efficacy in pre-registration nursing education. Nurse Education Today, 3(5), 405-410.
Schlairet, M. C., & Pollock, J. W. (2012). Equivalence testing of traditional and simulated clinical experiences: undergraduate nursing students’ knowledge acquisition. Journal of Nursing Education, 49(1), 43.
Schmidt, B., & Stewart, S. (2010). Implementing the virtual world of Second Life into community nursing theory and clinical courses. Nurse Educator, 35(2), 74.
Sears, K., Goldsworthy, S., & Goodman, W. M. The relationship between simulation in nursing education and medication safety. Journal of Nursing Education, 49(1), 52.
Sinclair, B., & Ferguson, K. (2009). Integrating simulated teaching/learning strategies in undergraduate nursing education. International Journal of Nursing Education Scholarship, 6(1), 1-11.
Steele, D. J., Johnson Palensky, J. E., Lynch, T. G., Lacy, N. L., & Duffy, S. W. (2002). Learning preferences, computer attitudes, and student evaluation of computerised instruction. Medical Education, 36(3), 225.
Sulivan-Mann, J., Perron, C. A., & Fellner, A. N. (2009). The effects of simulation on nursing students’ critical thinking scores: A quantitative study. Newborn & Infant Nursing Reviews, 9(2), 111-116.
Vivien, W. X., Tham, L. K. C., Lau, S. T. L., Mei, T.-T. Y., & Kiat, T. K. (2010). An exploration of the critical thinking dispositions of students and their relationship with the preference for simulation as a learning style. Singapore Nursing Journal, 37(2), 25-33.
Wang, K. H., Wang, T. H., Wang, W. L., & Huang, S. C. (2006). Learning styles and formative assessment strategy: Enhancing student achievement in Web-based learning. Journal of Computer Assisted Learning, 22(3), 207-217.
Yeager, S. T., & Gotwals, B. (2010). Incorporating high-fidelity simulation technology into community health nursing education. Clinical Simulation in Nursing, 6(2), e53.







