Design and Evaluation of a Conceptually-Based Home Telecare Program: Findings from a Mixed Methods Pilot Study
By: Donna Goodridge, RN, PhD (Corresponding Author)
College of Medicine, University of Saskatchewan
Saskatoon, SK, S7N 0W8
donna.goodridge@usask.ca
Phone 306-844-1469
Darcy Marciniuk, MD, FRCPC
College of Medicine, University of Saskatchewan
Saskatoon, SK, S7N 0W8
darcy.marciniuk@usask.ca
Brittany Kachur, RN, BScN, MPH, CRE
Chronic Disease Management Program
Saskatoon Health Region
brittany.kachur@saskatoonhealthregion.ca
Dana Higgins, RN, BN
Chronic Disease Management Program
Saskatoon Health Region
dana.higgins@saskatoonhealthregion.ca
Sheila Achilles, RN, MN
Director, Primary Health and Chronic Disease Management
Saskatoon Health Region
Sheila.achilles@saskatoonhealthregion.ca
Key words: telehealth, COPD, technology acceptance model, logic model
ABSTRACT
 Background: Home telecare (HTC) is changing the paradigm of service delivery for people living with long-term conditions, although the conceptual basis for this intervention is still evolving.
Background: Home telecare (HTC) is changing the paradigm of service delivery for people living with long-term conditions, although the conceptual basis for this intervention is still evolving.
Objective: The objective of this conceptually-based project was to better understand key elements of HTC and the ways in which it contributed or did not contribute to program outcomes in the unique context of a program for people with COPD located in Saskatchewan, Canada.
Methods: This mixed methods pilot study of an HTC intervention was guided by the Modified Technology Acceptance Model (MTAM) as well as the concepts of relationships, fit and visibility. Validated measures of quality of life, patient activation, functional status and patient satisfaction were used to evaluate outcomes. Qualitative interviews provided data on the patient experience.
Results: Thirty-two patients aged 48-91 completed the program. Findings confirmed the feasibility of the protocol and demonstrated high levels of participant satisfaction. A logic model was developed to diagrammatically represent the intervention.
Discussion: Use of the MTAM allowed for the focused collection of relevant data. The concepts of relationships, fit and visibility provided an analytical framework for the analysis of qualitative data. To fully harness the capabilities of HTC within local contexts, key issues such as interoperability of components, integration of telehealth data with the electronic medical record and data sharing amongst providers must be addressed.
Conclusion: Acceptance of technology in this study was high. HTC can alter the networks of relations and responsibilities between patients and provider and has substantial implications for workflow.
Introduction
Interest in clinical system re-design innovations is at an all-time high, given constraints in health care funding and an aging population. Home telecare (HTC) is changing the paradigm of service delivery for people living with long-term conditions and has the potential to improve patient and system outcomes. Evidence, however, regarding the effectiveness of HTC programs for people with chronic illness remains inconclusive. This has been compounded by significant heterogeneity in reported interventions and outcomes, (Bolton, Waters & Peirce, et al, 2011; Henderson, Knapp & Fernandez, et al, 2013; Polisena, Tran & Cimon, et al, 2010; Cruz, Brooks & Marques, 2014; Pinnock, Hanley, & McCLoughan, et al. (2013); McLean, Sheikh & Cresswell , et al. (2013), May, Finch & Cornford, et al. (2011) and a failure to adequately describe the intervention itself (Sheikh & Cresswell , et al. (2013). May and colleagues (2011) described the key barriers to integration of HTC as “uncertainties about coherent and sustainable service and business models; lack of coordination across social and primary care boundaries, lack of financial or other incentives to include telecare within primary care services; a lack of a sense of continuity with previous service provision and self-care work undertaken by patients; and general uncertainty about the adequacy of telecare systems” (p. 131).
HTC is an inherently complex intervention, with multiple components that must interact to produce intended results in outcomes and behavior (Moore, Audrey & Barker, et al. (2014); Barlow, Bayer & Curry (2006). HTC simultaneously engages with multiple actors (e.g. patients, families, clinicians; technology personnel and vendors; policy makers); objects (e.g. HTC systems; electronic health records) and contexts (health care delivery systems; rural, remote and urban settings). Complex interventions are deliberately initiated (institutionally sanctioned, formally defined; consciously planned and intended to lead to a changed outcome) attempts to introduce new or modify existing patterns of collective action (May, Finch & Ballini, et al, 2011).
There is increasing recognition of the value of understanding both the discrete components of complex interventions and the assumptions that purport to explain why an intervention is effective or not. Understanding how and why the intervention is “supposed to work” strengthens the design of the intervention itself and ensures congruence between the outcomes to be measured and the intervention (Craig, Dieppe & MacIntyre, et al, 2008). Improved theoretical understanding of how HTC can lead to improved outcomes allows weak links in the causal chain to be identified and strengthened. A better appreciation of the components of implementation of HTC interventions can also circumvent implementation failures in future applications (May, Finch & Ballini, et al, 2011).
This paper describes the development and evaluation of a conceptually-based HTC and support intervention for people with Chronic Obstructive Pulmonary Disease (COPD) in Saskatchewan, Canada, and reports on the learning from a pilot study. In addition to evaluating the HTC protocol and obtaining efficiency metrics for future costing and projections to inform subsequent studies, the aim of this project was to better understand key elements of HTC and the ways in which they contributed or did not contribute to program outcomes.
Methods
This three month mixed-methods pilot study was conducted between August, 2014 and January, 2015. Ethical approval was obtained from the University of Saskatchewan (Bio 14-147) and operational approval was obtained from the Saskatoon Health Region.
Participants and Recruitment
Eligibility criteria for this pilot project were: a) a spirometry-confirmed diagnosis of COPD (CTS Guidelines) (Thabane, Ma & Chu, et al, 2010) and b) meeting the criteria for enrollment in the LiveWell COPD Program (O’Donnell, Aaron & Bourbeau, et al, 2007). This program excludes people with COPD who: are palliative; have significant primary cardiac disease or lung cancer; are unable to provide informed consent; or reside in a personal care home or long-term care facility. Specifically for this project, other patients excluded were those with hearing or visual impairment that would preclude use of the HTC equipment. COPD Nurse Clinicians identified potentially eligible patients from the existing roster of the LiveWell COPD program as well as patients newly referred to the program.
Measures
The feasibility of using validated questionnaires that addressed key patient-oriented outcomes of interest was evaluated. Disease-specific quality of life was assessed using the St. George’s Respiratory Questionnaire (Saskatoon Health Region, 2010); patient knowledge, skill and confidence for self-managing using the Patient Activation Measure (Jones, 2009; Hibbard, Stockard, Mahoney & Tusler, 2004; Hibbard, Mahoney, Stockard & Tusler, 2005; Hibbard, Mahoney, Stock. & Tusler, 2007); generic health related quality of life using the CDC HRQOL-14 Health Days measure (Centers for Disease Control and Prevention, 2011); and self-reported health/functional status using the EQ-5D-3L Descriptive System (EuroQol, 2015).. Patient experience with HTC was evaluated using a modified version of the Telemedicine Satisfaction and Usefulness Questionnaire (TSUQ) (Bakken, Grullon-Figeruos & Izquierdo, et al, 2006).
Baseline assessment
After informed consent was received, baseline clinical data were obtained from the participant’s health record by the COPD Nurse Clinicians. A trained research assistant administered the self-report measures over the telephone.
HTC Intervention
The Intel-GE Care Innovations Health Guide TM HTC system consisted of: a home-based device (tablet with a touch screen interface), associated peripherals (oximetry, blood pressure) and a clinical care management application with customizable educational modules. It used a Bluetooth-enabled measurement device paired with the Health Guide, enabling wireless data transfer of biometric measurements. Data were hosted on a GE Care Innovations server.
The LiveWell COPD Team consisted of five COPD Nurse Clinicians (primarily Certified Respiratory Educators), the Program Manager and a Respirologist Medical Director. Two of the COPD Nurse Clinicians were designated as Virtual Care Nurses (VCNs) and assumed responsibility to develop educational content for the daily health sessions and for daily patient monitoring in the HTC program. For this project, a university-based researcher, graduate student research assistant, an Intel-GE product specialist and a representative from a home oxygen company completed the team. Community-based respiratory therapists employed by the home oxygen company delivered services related to: equipment asset management; commissioning; installation; training of participants and family on the use of the equipment as well as in-home technical support.
Following the in-person baseline assessment, monitoring equipment was installed in the patient’s home and instruction provided to the patient and family. Biometric data (pulse, blood pressure, and oximetry) was monitored daily (Monday to Friday) for the first eight weeks, decreasing to three times weekly for the last four weeks of short-term monitoring in cases where clinical stability was established. For all participants, the frequency of monitoring could be increased at the discretion of the VCN based upon the individual’s health status. Individualized thresholds for biometric and self-report data were set by the VCN, who received email notification of out-of-range values for telephone follow-up. In addition to monitoring biometric data, the VCN provided individualized support and follow-up. Participants were provided with contact information for both the monitoring nurse and equipment personnel. Figure 1 adapts a diagram produced by Rice (2011) and illustrates the core elements of the HTC intervention.
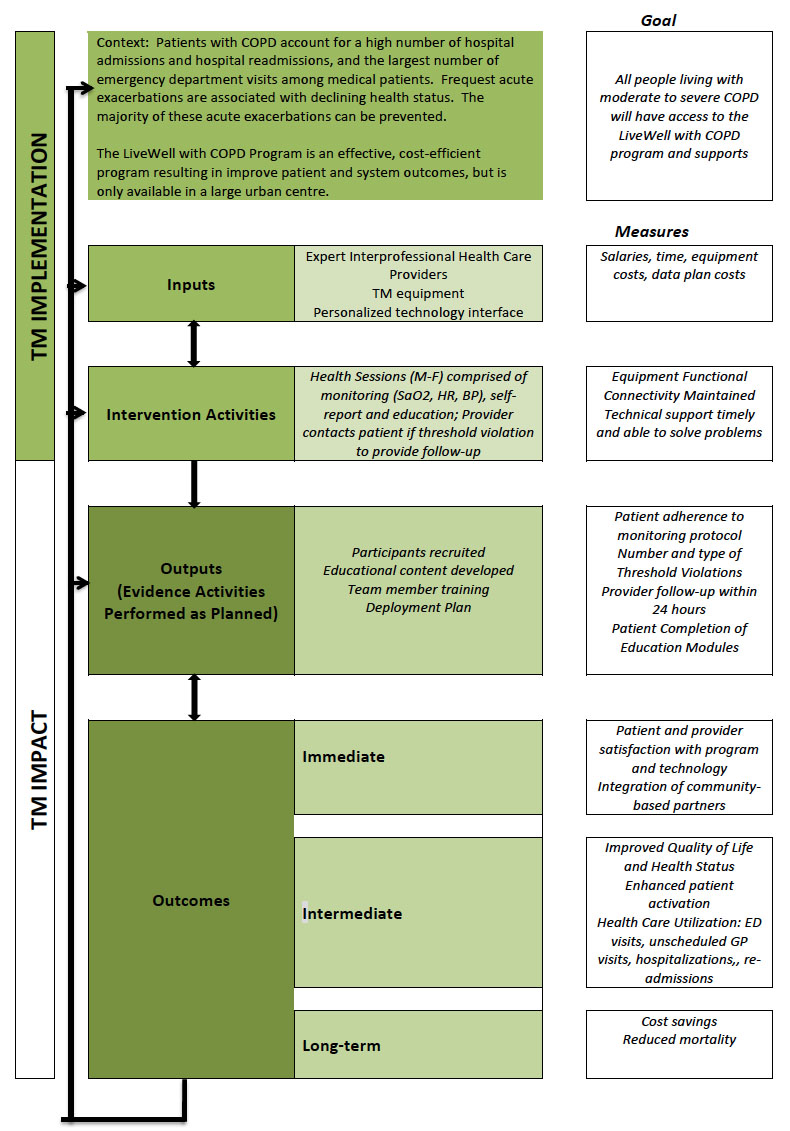
A logic model (Figure 2) was developed to diagrammatically represent the intervention and to describe anticipated delivery mechanisms (i.e. how resources will be applied to ensure implementation), intervention components (what is to be implemented), the mechanisms of impact (how the intervention will work) and intended outcomes (Moore, Audrey & Barker, et al, 2014).
The VCNs worked closely with the Lung Association of Saskatchewan to develop an 11 week program of educational content delivered daily in small doses following the transmission of biometric data. After transmitting biometric data (oximetry, pulse and blood pressure), the participant was asked a self-report symptom question. These questions related to: unscheduled health care visits, exercise, vaccinations and anxiety. Alerts were triggered to notify the VCN in the event that patients reported a notable change in status such as increased anxiety or increased shortness of breath.
The educational content focused on key areas of COPD and general wellness including medications, energy conservation, anxiety and exercise. Videos were used to augment content relevant to the week’s educational focus. Pre- and post-educational session knowledge questions were incorporated to allow for self-assessment and a motivational quote of the day concluded the session.
Theoretical Considerations
Because we were particularly interested in the patient experience of using the HTC system, our evaluation was guided by elements of the modified Technology Acceptance Model (McFarland & Hamilton, 2006) as well as by the mechanisms likely to ensure success of a HTC program proposed by Vassilev and colleagues (2015) in their realist review.
The original Technology Acceptance Model (TAM), based on the Theory of Reasoned Action (Fishbein & Ajzen, 1975), was developed by Davis, Bagozzi & Warshaw, 1989) and suggests that the acceptability of an information system is determined by two key factors: perceived usefulness and perceived ease of use. This theory was later modified by McFarland and Hamilton (2006). The modified model assumes that six contextual variables (prior experience; others’ use; computer anxiety; system quality; task structure; and organizational support) affect system usage through three mediating variables (computer efficacy, perceived ease of use, and perceived usefulness).
Three key concepts emerged from the realist review (Vassilev, Roswell & Pope, et al., 2015) that provided insights into the ways in which a HTC program might work: relationships, fit, and visibility. Given the centrality of the patient-provider relationship in the management of long-term conditions, HTC was considered to have the potential to establish new sources of connection by restructuring and re-shaping relationships. The fit between the HTC program and patients’ needs, environments, skills, capacity and daily lives also were viewed as potentially contributing to program success. Telehealth interventions that could be easily integrated into daily life and were easy to use were found by Vassilev and colleagues (2015) to be most effective. Finally, visibility, or visualization of symptoms and feedback, could improve knowledge, motivation and a sense of empowerment; engage network members; and reinforce positive behavior change, prompts for action and surveillance.
Quantitative Data Collection
Clinical data was obtained from patient health records. Participant self-report questionnaires were administered by telephone upon intake to the study and were repeated within two weeks of completing the three month HTC program. Clinician and manager questionnaires were completed one month following study closure. The research assistant entered Data into SPSS v. 22 and a 10 per cent random sample was checked for accuracy by a researcher (DG).
Qualitative Data
The qualitative interview guide for patients was developed to augment the data obtained through the Telemedicine Satisfaction and Usefulness Questionnaire (Bakken et al, 2006) and was based on key concepts from the TAM and realist review theories (Vassilev et al., 2015). Audiotaped telephone interviews of all participants were conducted by a trained research assistant following discharge from the program to explore their perceptions of the utility, benefits and challenges of using HTC. The interviews were transcribed verbatim. Face-to-face interviews were conducted with the VCNs to supplement the data obtained from the survey.
Sample Size and Statistical Analyses
While sample size calculations are not required for pilot studies (Hsieh & Shannon, 2005), our sample was considered sufficient to address our aims and representative of the target study population.
Data Analysis
Descriptive statistics were used to analyze the questionnaire results and establish a profile of participants. Using directed content analysis (Campbell, Murray. & Darbyshire et al., 2007) interviews were coded (DG) using Atlas.ti qualitative data management software. Members of the team reviewed and confirmed the coding.
RESULTS
Recruitment
Beginning in August, 2014, 52 eligible patients were pre-screened for eligibility from the roster of new referrals and existing patients from the LiveWell COPD Program and approached by the COPD nurse clinicians to participate in the program. Eight refused due to: a) being unfamiliar with the technology and not wanting to learn; or b) being “too busy”.
Eight of the remaining 44 declined at the time they were contacted for enrollment for the same reasons as above. The recruitment rate using COPD nurse clinician enrolment was 69.3%. Four patients withdrew due to illness or absence during vacation. A total of 35 patients were enrolled in and completed the three month program. One individual completed the program but declined to participate in the post-program evaluation.
Baseline Characteristics
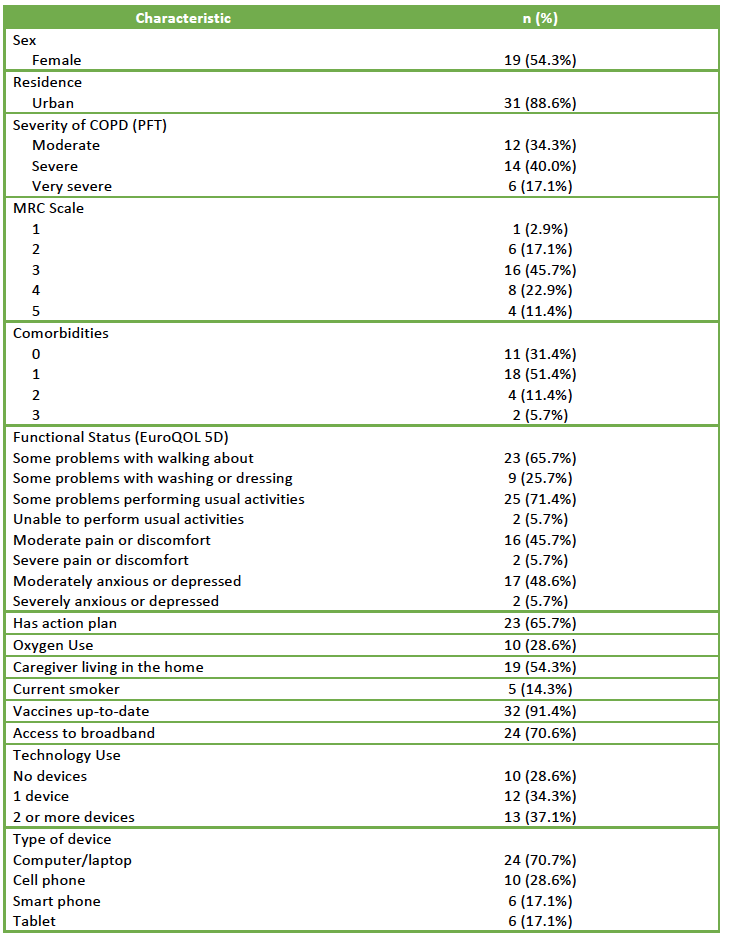
A profile of participant characteristics is provided in Table 1. Participants ranged in age from 48-91 years with a median age of 71 years (IQR=19).
Feasibility of the Protocol
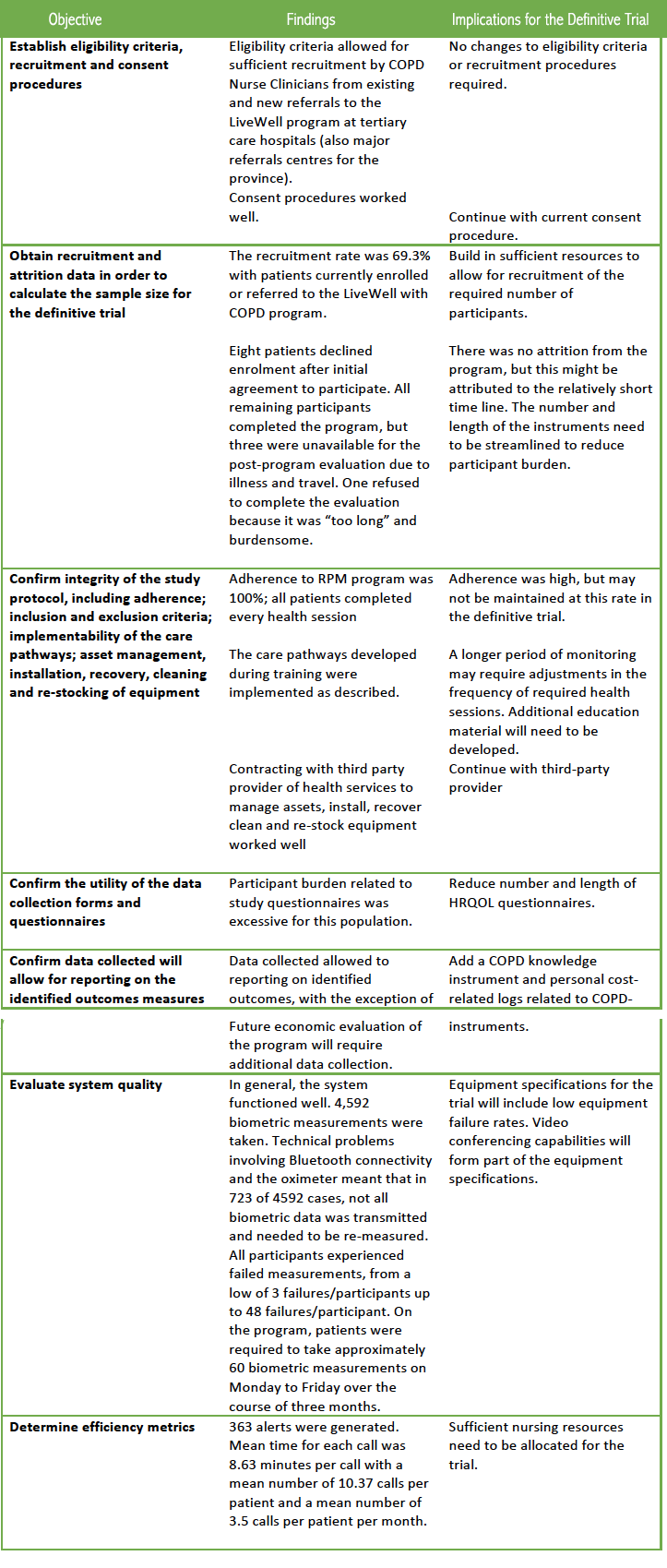
Table 2 addresses the research questions related to feasibility of the protocol. Other than alterations in the instruments used to collect the data, the protocol was deemed feasible for the subsequent clinical trial.
Acceptability of the HTC Intervention
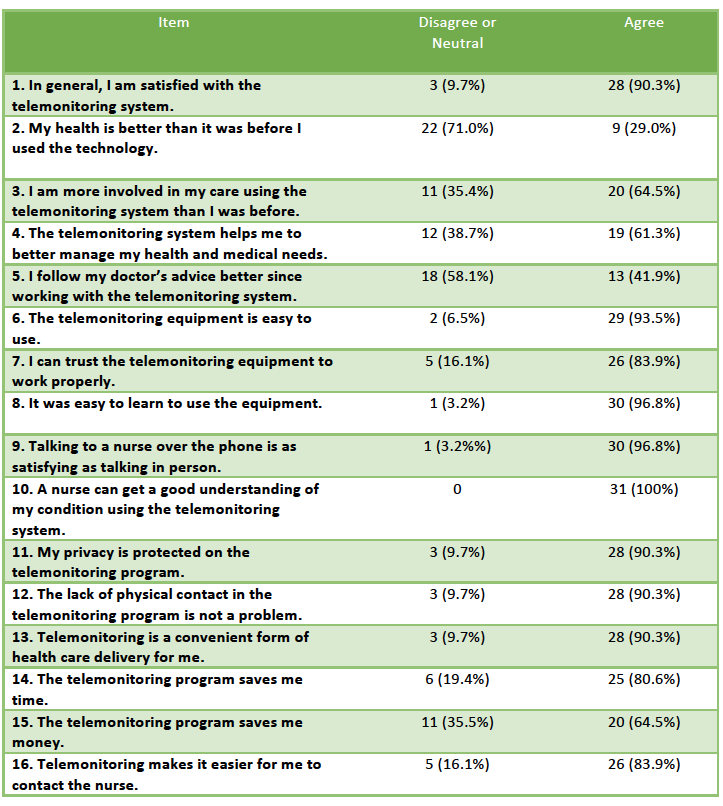
High levels of participant satisfaction with the HTC intervention were found on the TSUQ and confirmed by the qualitative interviews. Table 3 describes the levels of agreement with statements of usefulness.
Qualitative Findings
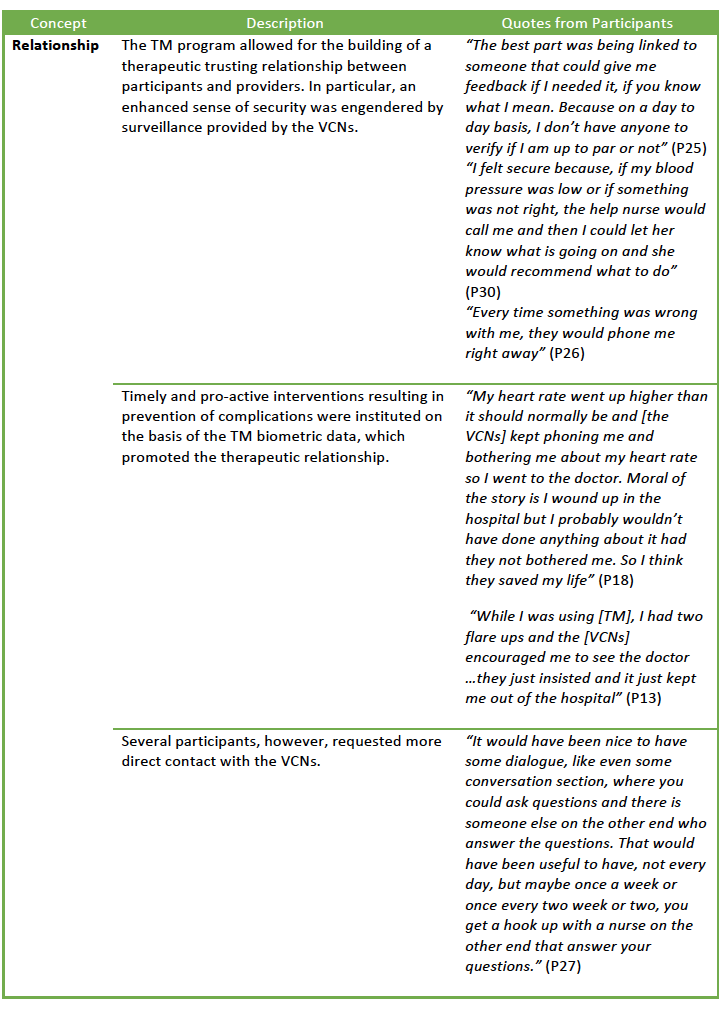
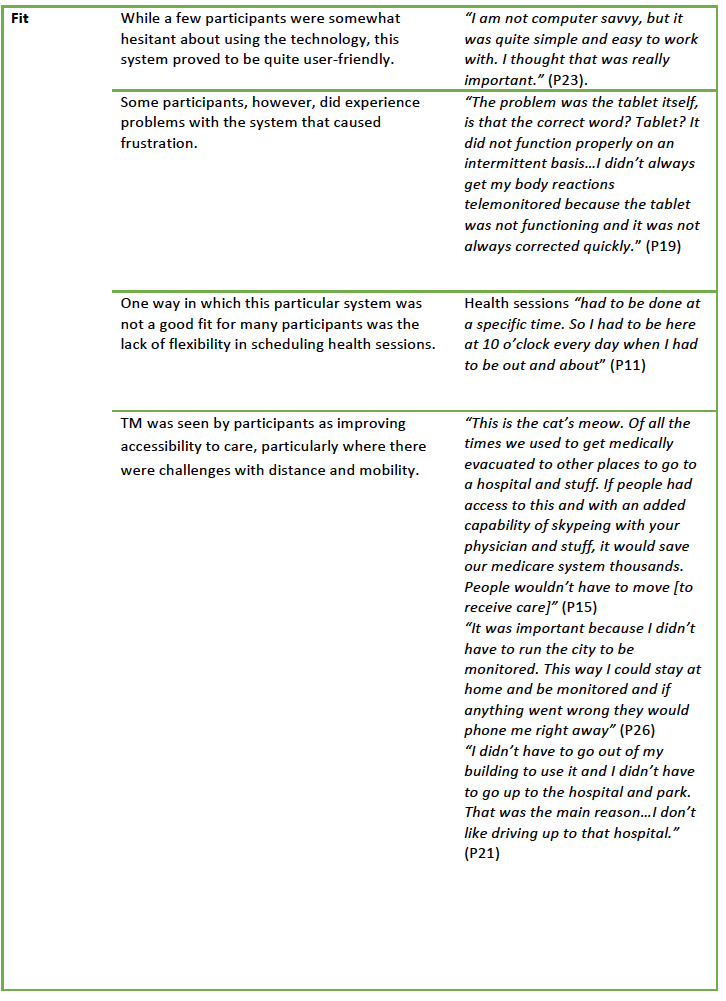
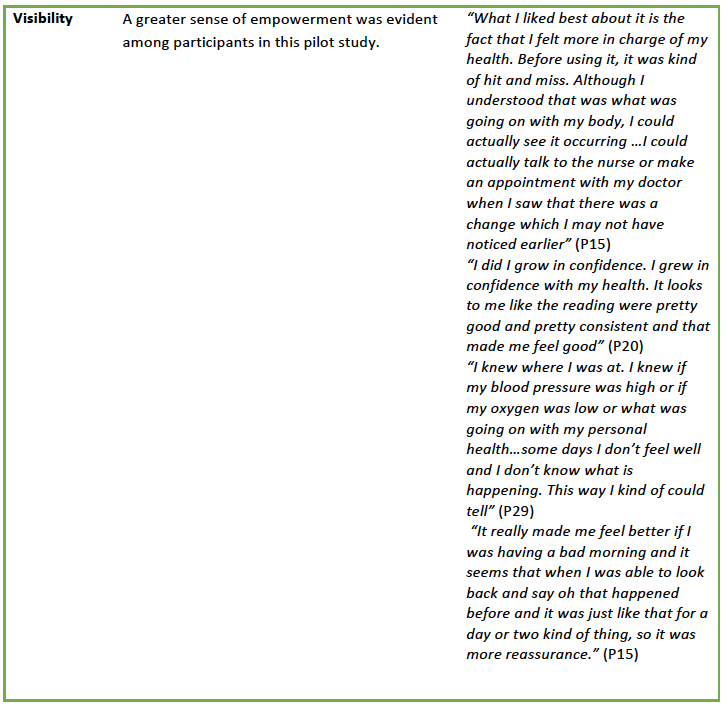
The qualitative data supported and supplemented the results of the TSUQ and provided additional insights into the patient experience of engaging in the HTC program. Findings were categorized according to Vassilev and colleagues’ (2015) key concepts of relationships; fit; and visibility (Table 4).
DISCUSSION
Main Findings
Acceptance of HTC was high among the participants of this study, as was hypothesized by the Modified Technology Acceptance Model (Bakken et al, 2006). While the majority (70%) of participants owned computers or smart phones, suggesting a basic level of computer efficacy, even those who did not own these devices report perceived ease of use of the system. The perceived usefulness of the system to participants was a key-mediating feature of acceptance, particularly in terms of the enhanced surveillance, earlier detection of health issues and ongoing connection to providers.
The concepts (relationships; fit and visibility) generated in the realist review of telehealth interventions (Vassilev et al., 2015) provided a robust framework for drawing themes from the qualitative data. Building relationships between user and providers through ongoing social interaction and support emerged as a key element of telecare in co-design workshops (Cruz, Brooks & Marques, 2014). HTC altered the networks of relations and responsibilities between patients and providers. Participants provided specific examples of the ways in which relationship, fit and visibility affected their personal experiences with HTC. In particular, enhanced surveillance and connection to providers provided a sense of reassurance that was highly valued by participants.
The role of patient activation (Jones, 2009; Hibbard, Stockard, Mahoney & Tusler, 2004; Hibbard, Mahoney, Stockard & Tusler, 2005; Hibbard, Mahoney, Stock. & Tusler, 2007) (having the information, motivation and behavioral skills necessary to self-manage chronic illness; collaborating with health care providers; maintaining functioning; and accessing appropriate care), may play an important role in HTC programs, but has yet to be fully explored. Different levels of activation may require programs with alternate foci and pace that better address the needs of individual patients.
Findings from the pilot study confirmed the feasibility of the eligibility criteria and the recruitment and consent procedures. The recruitment rate of 69.3% provides an important basis for planning recruitment for the definitive trial. The lack of attrition and 100% adherence might be attributable to the relatively short (3 month) time frame of the pilot study and may differ for a future definitive trial. Data collection using the specified questionnaires proved burdensome for some participants and alternative (and likely fewer) instruments for collecting key data will need to be considered. Because the HTC program included a substantial educational component, evaluation of participant knowledge will also need to be incorporated into the definitive trial protocol. Future economic evaluation will require the use of patient travel logs and health-care related expenses (e.g. accommodations for out-of-town medical appointments and tests). Participants were very positive about the HTC program and particularly appreciated the feedback on their health and the additional education.
While we reported no attrition from the HTC program and 100% adherence, attrition rates reported for other HTC studies varied from 0 to more than 20%; compliance rates of less than 80% were reported in some studies (Cruz, Brooks & Marques, 2014). In concordance with other studies, (Antoniades, Rochford & Pretto, et al., 2012; Chau, Lee & Yu,et al., 2012; Fairbrother, Pinnock & Hanley, et al., 2013; Fairbrother, Pinnock & Hanley, et al., 2012; Pinnock, Hanley & McCloughan, et al., 2013; Kim, Kim & Kim, et al., 2012) participants in the present study were very positive about using HTC, finding the system easy to learn and useful. Compared to the findings of Pinnock et al, (2013) the present study had a higher number of contacts per patient (2.1/month vs. 3.5/month). The number of contacts may be higher in the first few months of a HTC program as both patients and providers become accustomed to the system. The rate of alerts between these studies was not comparable due to the difference in study duration.
A significant finding was that the LiveWell COPD Program and team members were well positioned to undertake this pilot program. Their backgrounds and skills were appropriately utilized, although additional administrative and clerical support will be required for the main study in order to best utilize clinician expertise. A patient-focused HTC program requires an interdisciplinary team capable of dealing with the concomitant and complex challenges many patients with COPD face on a daily basis. These challenges may not be directly related to COPD, but have a significant impact on how well the patient is able to live with COPD. Greenhalgh and colleagues (2015) highlight the importance of using technology to digitally enable what “matters to the patient” (p.91). This demands a shift in focus that is less on the product and more on the support of technologies-in-use, which requires skilled human work, inter-sectoral negotiation and social infrastructure.
Strengths and Limitations
Deliberate incorporation of theoretical constructs from the TAM and the realist review allowed us to begin to describe the mechanisms by which HTC might achieve its goals of improving patient outcomes (Davis, Bagozzi & Warshaw, 1989) . Use of both interview data and self-report questionnaires allowed us to capture the key important features of the patient experience using this HTC program. A disciplined, systematic approach was used to design and pilot the HTC intervention.
There were relatively few participants from rural and none from remote areas in this study. Given that HTC can potentially improve accessibility to chronic disease management for patients in these settings, further work is needed to deal with the unique constraints inherent in these environments. Additional study of patients who declined enrollment will help to identify patient phenotypes for whom HTC may not work. In terms of planning for a future trial, recruitment rates may be lower when the intervention is rolled out across a wider range of settings (Moore et al, 2014).
Conclusions
This project has laid the groundwork for a large-scale trial of HTC for patients with COPD in a Canadian urban setting. To fully harness the capabilities of HTC across health care settings and between formal and informal caregivers, key issues such as interoperability of components, integration of HTC data with the electronic medical record and data sharing amongst providers must be addressed.
Acknowledgements
We wish to thank the participants in this study, who gave generously of their time and allowed us to complete this pilot project. The authors acknowledge the invaluable assistance of Andrew Bennett in data collection and the generous support of the Saskatoon Health Region.
Funding Acknowledgement
We acknowledge the financial support and expertise provided by Canada Health Infoway.
Contributions
DG and DM were the originators of this project, developed study design, secured funding, provided study administration, data analysis, interpretation of results and writing of the paper. BK, DH and RS participated in the design of the project. BK and DH led the implementation of the project. DG wrote the initial draft of the paper and all authors contributed to the final version.
Competing Interests
The authors have no competing interests.
References
Antoniades, N.C., Rochford, P.D. & Pretto, J.J. et al. (2012). Pilot study of remote telemonitoring in COPD. Telemedicine Journal and e-health,18(8),674-682.
Bakken, S., Grullon-Figeruos, L. & Izquierdo, R. et al. (2006). Development, validation and use of English and Spanish versions of the Telemedicine Satisfaction and Usefulness Questionnaire. Journal of the American Medical Informatics Assocation,13, 660-667.
Barlow, J., Bayer, S. & Curry, R. (2006). Implementing complex interventions in fluid multi-stakeholder environments: experiences of telecare. Technovation, 26, 396-496.
Bolton, C.E., Waters, C.S., Peirce, S., et al., on behalf of the EPSRC and MRC Grand Challenge Team. Insufficient evidence of benefit: a systematic review of home telemonitoring for COPD. (2011). Journal of Evaluation in Clinical Practice, 17(6), 1216-1222.
Campbell, N.C., Murray, E. & Darbyshire, J. et al. (2007). Designing and evaluating complex interventions to improve health care. BMJ, 334, 455.
Centers for Disease Control and Prevention. (2011). CDC HRQOL-14 “Healthy Days Measure”. Available at http://www.cdc.gov/hrqol/hrqol14_measure.htm.
Chau, J.P.C., Lee, D.T.F. & Yu, D.S.F., et al. (2012). A feasibility study to investigate the effectiveness of a telecare service for older people with chronic obstructive pulmonary disease. International Journal of Medical Informatics, 81(1), 674-682.
Craig, P., Dieppe,P. & MacIntyre, S. et al. (2008). Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ, 337, a1655.
Cruz, J, Brooks, D. & Marques A. (2014). Home telemonitoring in COPD: a systematic review of methodologies and patients’ adherence. International Journal of Medical Informatics, 83(4), 249-263.
Davis, F., Bagozzi, R. & Warshaw, R. (1989). User acceptance of computer technology: a comparison of two theoretical models. Management Science, 35(8), 982-1003.
EuroQol. (2015). How to use EQ-5D. Available at http://www.euroqol.org/about-eq-5d/how-to-use-eq-5d.html.
Fairbrother, P., Pinnock, H. & Hanley, J. et al. (2013). Exploring telemonitoring and self-management by patients with chronic obstructive pulmonary disease: a qualitative study embedded in a randomized controlled trial. Patient Education and Counseling, 93(3):403-410.
Fairbrother, P., Pinnock, H. & Hanley, J. et al. on behalf of the TELESCOT programme group. (2012). Continuity, but at what cost? The impact of telemonitoring COPD on continuities of care: a qualitative study. Primary Care Respiratory Journal, 21, 322-328.
Fishbein, M.A. & Ajzen, I. (1975). Belief, attitude, intention and behavior: an introduction to theory and research. Reading, MA: Addison Wesley.
Greenhalgh, T., Procter, R. & Wherton, J. et al. (2015). What is assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Medicine,13, 91.
Greenhalgh, T., Procter, R. & Wherton, J. et al. (2015). What is assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Medicine,13, 91.
Henderson, C., Knapp, M., Fernandez, J.L., et al. (2013). Cost effectiveness of telehealth for patients with long-term conditions (Whole Systems Demonstrator telehealth questionnaire study: nested economic evaluation in a pragmatic, cluster, randomized controlled trial. BMJ, 346;f1035.
Hibbard, J.H., Mahoney, E.R., Stock, R. & Tusler, M. (2007). Do increases in patient activation result in improved self-management behaviors? Health Research & Educational Trust, 24(4), 1443-1463.
Hibbard, J.H, Mahoney, E., Stockard, J. & Tusler, M. (2005). Development and testing of a short form of the Patient Activation Measure (PAM). Health Services Research 40(6), 1918-1930.
Hibbard, J.H., Stockard, J., Mahoney, E. & Tusler, M. (2004). Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research Journal, 39, 1005-1026.
Hsieh, S. & Shannon. S.E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277.
Jones, P. (2009). St. George’s Respiratory Questionnaire Manual. St. George’s University of London. Available at http://www.healthstatus.sgul.ac.uk/SGRQ_download/SGRQ%20Manual%20June%202009.pdf.
Kim, J., Kim, S. & Kim, H.C. et al. (2012). Effect of consumer-centred u-health service for the knowledge, skill and attitude of the patients with chronic obstructive pulmonary disease. Computers, Informatics in Nursing, 30(12):661-71.
May, C.R., Finch,T.L, Cornford, J, et al. (2011). Integrating telecare for chronic disease management in the community: What needs to be done? BMC Health Services Research, 11:131.
May, C.R, Finch, T. & Ballini, L. et al. (2011). Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMC Health Services Research,11, 245.
McFarland, D.J. & Hamilton, D. (2006). Adding contextual specificity to the technology acceptance model. Computers in Human Behavior, 22, 427-447.
McLean S, Sheikh A, Cresswell K, et al. (2013). The impact of telehealth on the quality and safety of care: A systematic overview. PLOS ONE, 8(8), e71238.
Moore, G., Audrey, S., Barker, M. et al. (2014). Process evaluation of complex interventions: Medical Research Council guidance. MRC Population Health Science Research Network, London.
O’Donnell, D.E., Aaron, S. & Bourbeau, J. et al. (2007). Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2007 update. Canadian Respiratory Journal, 14(Suppl B), 5B-32B.
Pinnock H, Hanley H, McCLoughan L., et al. (2013). Effectiveness of telemontioring integrated into existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: researcher blind, multicenter, randomized controlled trial. BMJ, 347, f6070.
Polisena, J, Tran, K, Cimon, K, et al. (2010). Home telehealth for chronic obstructive pulmonary disease: a systematic review and meta-analysis, Journal of Telemedicine and Telecare, 16(3), 120-127.
Rice P. (2011). Telemonitoring for long-term conditions: A workbook for implementing new services models. Available at http://yhhiec.org.uk/wp-content/uploads/2011/10/11070604_Tele_Moni_Workbk.pdf.
Saskatoon Health Region. (2010). 2009-2010 Annual Report. Available at http://www.finance.gov.sk.ca/paccts/paccts10/compendium/reports/hcSaskatoon
Thabane, L., Ma, J. & Chu, R. et al. (2010). A tutorial on pilot studies: the what, why and how. BMC Medical Research Methodology,10, 1.
Vassilev, I., Roswell, A. & Pope, C. et al. (2015). Assessing the implementability of telehealth interventions or self-management support: a realist review. Implementation Science, 10,59.
Image Credit
Medical graphic by Freepik from Flaticon is licensed under CC BY 3.0. Made with Logo Maker
AUTHOR BIOS
Donna Goodridge is a Registered Nurse and Professor in the College of Medicine at the University of Saskatchewan. Her research interests include health services improvement and patient engagement, particularly for people living with chronic illness.
Darcy Marciniuk is the Acting Vice-President of Research at the University of Saskatchewan and a practicing respirologist in Saskatoon. He is the Medical Director for the LiveWell with COPD program with the Saskatoon Health Region. His research focuses on COPD and includes clinical pathways for this population.
Brittany Kachur and Dana Higgins are COPD Nurse Clinicians with the LiveWell with COPD Program in the Saskatoon Health Region. Brittany and Dana served as the Virtual Care Nurses for this project.
Sheila Achilles was the Program Director for the Chronic Disease Management Program in the Saskatoon Health Region during this project and has since retired.