Electronic Health Records in my Unit? … No Thanks!: A Qualitative Research Project using Extreme Case Sampling
by Wendy Seidlitz, RN, BScN, MSc, Clinical Informatics Specialist*
Dr. Susan Blatz, RN, MEd, PhD, Clinical Nurse Specialist*
Barb Jennings, RN, MSHSA, Program Manager*
Rebecca LaRocca, RN, BScN, MSc, Registered Nurse*
*McMaster Children’s Hospital, Hamilton Health Sciences, 1200 Main St. West
Hamilton, Ontario, Canada, L8N 3Z5
Abstract
Electronic health records are being implemented in many hospitals across Canada, yet there is a small group of nurses who would rather quit or retire than be working in their unit prior to implementation of electronic health records. This qualitative research study used extreme case sampling to reveal the thoughts, opinions and needs of these nurses. The ten themes that arose were: resource needs, change and transition, documentation, technology, nursing roles, diminished caring, computer literacy, positive comments, generations and negative comments. When these themes were triangulated with the opinions of the participants’ formal and informal leaders, the analysis was confirmed as valid. The revealed themes and sub-themes will serve as excellent valid evidenced-based indicators for use in quantitative survey tools during future electronic health records research.
Key Words
Electronic Health Records, Qualitative Research, Nurses, Extreme Case Sampling
Introduction
Hospitals are moving from paper documentation towards Electronic Health Records (EHRs) with the goal to support continuing, efficient and quality integrated health care. Nurses have voiced their concerns about EHRs and the significant change in nursing that computerization has brought to the profession, but have they been heard? The goal of this research is to reveal the thoughts, opinions and needs of nurses who may be feeling that they wish to leave the nursing workforce early because of the movement towards EHR documentation. Understanding the thoughts and opinions and listening to the needs of nurses is essential for supporting all nurses during the transition to EHRs.
Background /Significance
Implementing an EHR system is a complex change management process fraught with risk and conflict that requires careful strategic planning (McLane 2005; Kaufman Roberts, Merrill, Lai & Bakken, 2006). There is consensus, if not consistent empirical evidence, that the adoption of EHR systems can improve patient care, reduce risks to patients due to error, and improve legibility, security and cohesion of health care records. Although it was thought that EHRs would save time, this has yet to be proven by research (Poissant, Pereira, Tamblyn & Kawasumi, 2005). A recent literature review concluded that some nurses are dissatisfied with the state of the electronic health records (Stevenson, Nilsson, Petersson& Johansson,2010). It is becoming clear that some nurses are having difficulty with computers and the implementation of EHRs (Lee, 2007). A few of these nurses confess, in essence, they would rather retire or leave their job than be working in their unit when EHRs are implemented.
In 2009, the average age of Canadian nurses was 45.2 years with the top four age groups clustered at or above 40 years (Canadian Institute for Health Information, 2010). National projects are underway in Canada aimed specifically at recruiting and retaining nurses (Canadian Federation of Nurses Unions, 2012). It is important to listen to and understand issues that are critical to nurses to retain our existing nurses and recruit new ones.
Research Question and Theoretical Background
The impetus for this research question arose from the primary author’s personal experience while working as a clinical educator in a critical care area that did not yet have EHR. The primary author was aware of nurses who had stated they would avoid working in a unit that had EHR. This knowledge led to the final research question: “When registered nurses (RNs) agree with a statement that they would rather retire or leave their job than be working in their unit when EHRs are implemented, what processes and opinions are involved which lead them to agree with such a statement?”
The Theory of Planned Behaviour, a psychological theory which links attitudes to behaviour, was used to frame the research study (Ajzen, 1991). This theory may be valuable to explain the phenomenon of intention for ‘behavioural avoidance’. In this case, nurses may seek to avoid working on their units during the implementation of EHRs. The avoidance may be in the form of early retirement, job change to an institution without EHR or leaving the nursing profession. Since this research is exploratory, qualitative methodology was sought.
Methods – Phase 1
Qualitative research using a case study methodology was employed using extreme case sampling. Participants in Phase 1 of the study were Registered Nurses employed at the hospital where the study was being undertaken who agreed to statement “E” in our recruitment flyer. Statement E, representing the extreme case, was as follows: “I feel like I would rather retire or leave my job than be working in my unit when electronic health records are implemented.” Statements A though D represented more favourable opinions about EHRs. Thus, the authors felt that extreme case sampling would allow for efficient data collection revealing the most number of themes in the shortest possible time. There was no exclusion criteria provided the research participants met the criteria described above.
A research ethics board approved recruitment flyer was circulated to all areas of the multi-site hospital in order to solicit potential participants. Follow-up with managers and educators in the hospital units was done to ensure the flyers were posted and to improve awareness of the study. The study was also posted to the nursing intranet and was presented to the hospital research committee.
Eleven Registered Nurses (RNs) who worked in pediatric (N=6) and adult (N=5) nursing areas consented to be interviewed. All participants were between the ages of 35 and 65 and all had diplomas as their highest level of completed formal nursing education. Participant years of nursing experience ranged from: 5-9 years (N=1), 15-24 years (N=1), 25-34 years (N=5), and more than 34 years (N=4). Interviews were conducted away from the patient care area and lasted between 30 and 60 minutes. All interviews were semi-structured but allowed for further probing based on the answers provided (see Table 1). No incentives were offered to Phase 1 participants however parking fees were paid if they had been incurred. All Phase 1 interviews were completed over a 3 month time period. All eleven participants consented to be contacted one year from the date of their interview to determine if their opinion had in fact resulted in a change in employment.
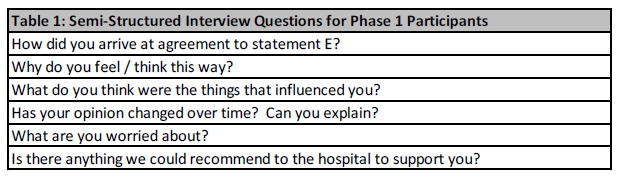
TABLE 1: Phase 1 Interview Questions
Methods – Phase 2
The Phase 2 interview process was developed to seek alternate opinions about why registered nurses might consider avoiding work in a unit where EHR is implemented. The research goal of Phase 2 was to increase the validity and credibility of the overall results through alternative data sources or triangulation (Halcomb, 2005). Potential Phase 2 participants were approached based on their role in a recent (within 6 months) involvement with local EHR implementation teams. Of the ten people approached, nine consented to participate. All nine were formal or informal leaders from wards, a critical care unit or clinical informatics teams. No Phase 2 participants were aware of the identities of the Phase 1 participants. Phase 2 participants agreed to share their thoughts about individuals who might feel like they would rather retire or leave their jobs rather than be working when EHRs are implemented. Nine semi-structured interviews (see Table 2) were completed over a five month time frame that began just as the Phase 1 interviews were being completed. All Phase 2 interviews were completed prior to thematic analysis of the Phase 1 interviews so as not to influence the Phase 2 interviews.
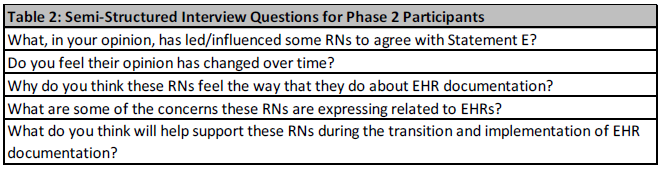
TABLE 2: Phase 2 Interview Questions
Data Analysis & Results
All Phase 1 & 2 audio-tapes were transcribed verbatim and irreversibly anonymized for circulation to the research team. All transcriptions were double checked with the original audio-tapes by the research team, and later destroyed. After the first few interviews were transcribed and analyzed, a code book of developing major and minor themes was created. The code book went through five iterations as new themes emerged, themes were combined, split, or moved. The final version of the code book is presented in Table 3.
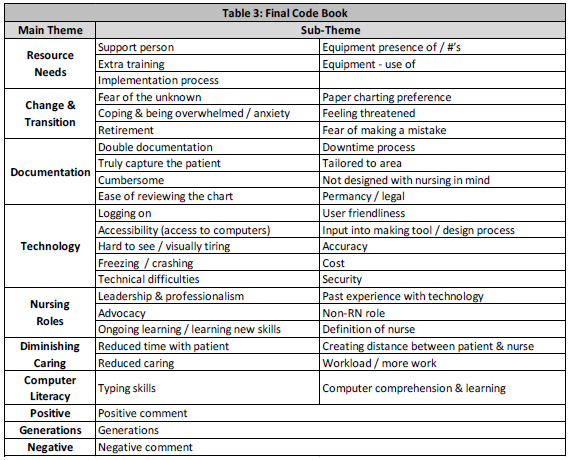
Table 3: Final Code Book
All four authors independently coded three Phase 1 and one Phase 2 interviews and then reached consensus on the thematic coding of those interviews. Disagreements that occurred were discussed until consensus was achieved. Next, all remaining interviews were independently coded by two of the authors, who then met and reached consensus on the thematic coding. A third author was consulted if consensus could not be reached.The research team used manual data analysis with a colour coding system representing each of the major themes and an alphabetical system representing the subthemes. Codes per interview were collated by interview phase (see Table 4). When coding the Phase 1 and Phase 2 interviews, the researchers also took care to highlight quotes from the participants which were particularly clear and representative of the theme in question.
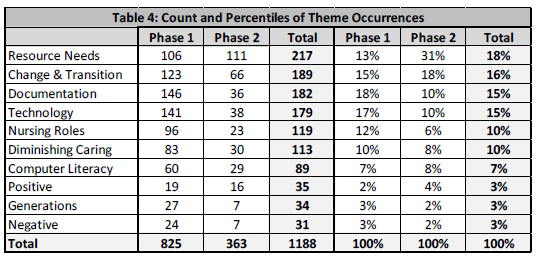
Table 4: Theme Occurrences
Thematic Analysis & Interpretation
All Phase 1 and Phase 2 interviews underwent thematic analysis using the code book presented in Table 3. A discussion follows about each of the ten major thematic categories. The discussion begins with the theme which was spoken about most often, when analyzed collectively by all 20 participants (as seen in Table 4). Differences in ranking between Phase 1 and Phase 2 participant’s responses have been highlighted.
All participant quotes have been anonymized by replacing potentially identifying references to unit type or patient type with generic terms (e.g. “patient”); these are identified for the reader in square brackets. Lastly, to allow improved understanding of the discussion context, descriptive details, also in square brackets, were added for clarity.
Resource Needs (Overall Rank = 1st)
Of the ten major themes revealed, the formal and informal leaders in Phase 2 spoke most often about how EHR implementation would impact on the resource needs of their area. Although Phase 1 participants described their resource needs less often than Phase 2 participants, they spoke about a need for extra training, a need for support personnel, and the presence of and use of the equipment itself.
“I should be able to page for a backup and expect that [the support person] should be able to come or call back at some point during the shift.” (Phase 1)
“We need a real learning period with it first. And then um, you know and everyone really needs to be comfortable with it before it, it becomes the, the legal record in a patients chart.” (Phase 1)
“Another thing they’re going to need to do is add more computers because there’s not enough computers for everybody” (phase 1)
“Like the doctor will come on and look something up. So he wipes you out then you gotta log back in and all the rest of the stuff. So, something that was specific to the individual for the day, everybody has their own.” (Phase 1)
“I think that the support when you go live, that it is um imperative and I think the support needs to be useful. I think that somebody needs to be on a pager or available – actually be on the unit.” (Phase 2)
“I think they [training staff] need to choose their time to come and do the teaching, when it’s very busy during peak times and different floors will have different peak times.” (Phase 2)
“I think probably the most important thing is listening and responding umm to what the nurses have to say uhh as we go through the project.” (Phase 2)
“I think that there needs to be this constant positive attitude. Um constant reinforcement that “yes” you’re bright enough to learn this. I mean look at all the skills you’ve learned over the last X amount of years of nursing. It’s just one more skill that I know you can do and I know that you can be good at because you’re good at everything else. So that kind of positive feedback that makes them feel good about them and their ability to learn something new.” (Phase 2)
Change & Transition (Overall Rank = 2nd)
All phase 1 participants were able to acknowledge their feelings about the change and transition that would occur in nursing, in their units and in themselves during the move to EHR documentation. The nurses discussed coping, anxiety & being overwhelmed, a fear of the unknown, a fear of making a mistake, and feelings of being threatened. They clearly stated their preference for remaining with paper charting and their preference for being retired or in an alternate setting prior to EHR implementation. Phase 2 participants commented on change & transition the second most often of all ten themes. They were clearly aware of the significant impact EHR implementation would have on the emotional and mental health of the nurses.
“There’s been so many changes over the past, ah, lifetime of nursing, but certainly the past ten years, the changes have been immense.” (Phase 1)
“It’s just it’s scary, it’s gonna be scary for us. It’s, it’s a lot of us who are older and not used to computers.” (Phase 1)
“I have to focus my energy on doing my job and thinking about what I am doing and then you add this on, on top of it and it is, um, overwhelming.” (Phase 1)
“I really thought I would, I would retire (laughing) before I had, I had to you know, I thought really I’d be gone before it [EHR implementation] was staring, staring me in the face thinking “Okay, you have to do this now” and I have been told many times. I, you have to do this, like, you can’t, you can’t stick your head in the sand.” (Phase 1)
“One of the other emotions is anxiety and sometimes the anxiety levels are so high that it defeats the ability to learn a new skill.” (Phase 2)
“Some of them had hoped it [EHR] would come along after they retired.” (Phase 2)
“Feeling the accountability of the magnitude of the responsibility if they don’t know how to push buttons on the computer.” (Phase 2)
“I think that it takes a lot of guts for someone to say ‘You know what I’m feeling, I don’t get this’ and ‘I don’t know if I can do this properly’, knowing that this is the way you have to do your job and there might be repercussions if you’re saying that.” (Phase 2)
Documentation (Overall Rank = 3rd)
Out of all the major themes revealed, Phase 1 nurses had the most comments about how EHR was going to impact on their documentation. Nurses worried that by using EHR they would be using a tool not designed for nurses, not designed for their nursing specialty area, or even one that was not able to truly capture the status of their patient. The Phase 1 nurses worried that the system would be cumbersome to use, would be difficult to review the chart for historical information, or that it would lead to double documentation. As well, they wondered about what would happen if the system was not functioning and whether or not the system was truly permanent (like their familiar paper system). They also had concerns about the legal ramifications of charting electronically. Phase two participants acknowledged these fears and were able to put themselves back in the nurses’ shoes occasionally sharing some similar concerns.
“You go to the bedside with your little piece of paper, you write down your vital signs, your assessment, and uh, everything you need and then you go back and you enter it all on the computer.”(Phase 1)
“We have the big flow sheets, I can look at that and I can see everything in a glance. I can keep all, I can look at all the threads that, that are that patient’s status. I can look at how things are trending. I can think “Oh, hold on”, you know, like you can join the dots of things that are happening.” (Phase 1)
“It doesn’t seem to flow, um, and therefore it’s difficult cause you end up with pages and pages of stuff that you have to review in order to extrapolate bits and pieces of information that you want.” (Phase 1)
“It isn’t designed very often with us [nurses] in mind. It’s designed for other people so then it becomes, if it’s not designed with us in mind, then it revolves around other people’s needs and to make other people’s lives easier and not, and not nursing’s lives easier.” (Phase 1)
“I think that probably right now that’s one of the biggest frustrations for many staff members is where to put some of the pieces of documentation that they had previously been able to put on their flow sheets.” (Phase 2)
“I think that there’s some level of frustration that they are finding, that they are writing certain things on a piece paper to be able to keep with them later, so they are thinking that this is kind of a waste of time. So, you know, they are doing the same task twice, they are writing it down on a scrap of paper and entering it into the keyboard.” (Phase 2)
“I think people are struggling with looking. They’re used to flipping through pages and I think they’re struggling with finding things in the computer” (Phase 2)
“They’re afraid that the patient’s documentation will be lost completely if something happens. They don’t understand all of the saving of the information” (Phase 2)
Technology (Overall Rank = 4th)
Technological concerns were the second most talked about issue brought up by Phase 1 participants. They mentioned that the computers themselves were a barrier to care due to freezing and crashing, the long log in times, the accessibility of the computers both in numbers and placement, and the visual difficulties encountered when trying to view EHRs on screen. They also were worried that the system would not be user friendly or accurate, that the system was costly or that it had been designed without enough input from front line nurses. Phase 2 participants were aware of these concerns and perceptions and some shared these concerns as well.
“I find it really hard on the eyesight. Umm…depending on what type of screen and that, I find it very like visually tiring.” (Phase 1)
“For nurses on the [unit], make it user friendly. Like you shouldn’t have to go screen to screen to screen. Everything should be on the one screen. It should be quick. You should be able to click, click, click, click, click and basically anything that you would want to chart should already be there.” (Phase 1)
“You know the management go and purchase these programs and by the time that any nurse gets to look at it, it’s way too late and it’s a done deal.” (Phase 1)
“I really worry about systems crashing and I have no paper work documentation.” (Phase 1)
“Having problems seeing the keyboard, having wearing bifocals and trifocals umm, they’re having trouble reading some of the flow sheets because they are so small.” (Phase 2)
“One of the concerns is it takes a long time for them to log in.” (Phase 2)
“Before people could chart and use their own terminology and their own words. Now it’s on a screen, so they have to understand those words.” (Phase 2)
“I think there’s some fear that some of the documentation that comes over isn’t going to be what they want or if they make a mistake, it’s there forever. And you know, not that people are nervous about making mistakes, but if something comes into a chart or it’s the wrong patient how do you fix that?” (Phase 2)
Nursing Roles (Overall Rank = 5th)
Phase 1 participants touched on a variety of matters related to their nursing role being impacted by EHR implementation. These included nursing advocacy, nursing leadership and professionalism, and the basic definition of a nurse. They also discussed how their nursing role was impacted by their ongoing learning, their past experience with technology and the influence of non-nursing roles. Phase two participants had less to say about nursing roles than Phase 1 nurses. This may be because they have already embraced EHR as part of the nursing role.
“I don’t think it’s even really our job per say. Our job is what I would like it to be, is at the bedside you know. And, and it’s certainly moving away from that, and it will even move further once this [EHR] here gets implemented too.”(Phase 1)
“You can fit in charting by paper anytime, anywhere. People see you, doing nursing care and nursing related things.” (Phase 1)
“I think they’re re-looking at any ways, at the structure of nursing and um, taking us away from the bedside, and giving a lot more of the, that work and that assessment to the health care aides and um, I just think it’s moving in the wrong direction.” (Phase 1)
“To me there’s only, there’s only one thing, and that’s the patient and the family. And that’s always been my agenda. It’s always been my priority, and it still is. And that’s never going to change for me, so I think anything else that, I, although I understand that other things have to come into play, that’s not, that’s not what it’s about for me. That’s why I went to school. That’s why I became a nurse. They are the most important thing, they should be, nothing else should matter except the patient and family.” (Phase 1)
“I think that people need to keep an open mind and understand that this is an iterative process. It is going to grow and change and get better and more robust. And, unfortunately, we do have to start somewhere.” (Phase 2)
“I think that documentation for nurses is a very personal thing. You take pride in it. You want to do it well. And I think their big issue is, is this going to demonstrate how I would do it and be as good as I would like it to be and as complete and as comprehensive and all of those things.” (Phase 2)
“One of the other issues is that they’re concerned that the physicians won’t do their part and will dump it on the nurses.” (Phase 2)
Diminished Caring (Overall Rank = 6th)
The Phase 1 participants commented about how EHR would diminish their ability to care for the patient by reducing the time they could spend with their patient, creating distance between themselves and the patient and by increasing their workload. The Phase 2 participants, all leaders in their EHR implementation, were able to similarly acknowledge the nurses’ concerns for their ability to provide patient care with these new challenges.
“My job, to me, is to support my [patient] and support my family and every time we add one more, whether it’s computer or not, it just chips away. And I still only have my 12 hours and it just chips away, and chips away, and chips away at me being able to give fabulous nursing care to people who need it… because I’m struggling with a computer or I’m collecting data for a government.” (Phase 1)
“When I went into nursing in the first place I didn’t go in to do a lot of electronic things. I was, I chose nursing because I wanted that uh, hands on, helping people and this just doesn’t quite feel like that.” (Phase 1)
“It’s [referring to EHR] going to take away from what I really want to do, which is, the patient care and dealing with the families and [patients]” (Phase 1)
“Workload can be a real concern because if you’ve got three or four [patients], you’ve got to do electronic charting on four [patients] and you’re not real comfortable with the system – it’s going to take you a long time.” (Phase 1)
“[They] worry that it’s [referring to EHR] going to take a lot of time away from your ability to give patient care” (Phase 2)
“It [referring to EHR] takes more time, there’s absolutely no doubt about it. It does take more time until you get used to it.” (Phase 2)
“If nurses had the choice between sitting down and documenting for half an hour or getting to do something for their patient, they would prefer doing something for their patient.” (Phase 2)
“They’re worried that the way that this sort of change will worsen their care, worsen their ability to uhh deliver excellent care for their patient.” (Phase 2)
Computer Literacy (Overall Rank = 7th)
Both Phase 1 and Phase 2 participants shared concerns about nurses typing skills, computer literacy, computer comprehension and ability to learn about the computer environment.
“I’m not fast at it [using a computer] because I haven’t done it all my life. It’s a thing that I had to learn. I still type with two fingers.” (Phase 1)
“I am computer illiterate. I know how to check my emails and that is about it.” (Phase 1)
“So people who aren’t good at typing, or very good in computers at all, and you’ve had a busy assignment – you’re going to be there past your shift, inputting all your information.” (Phase 1)
“Some people maybe haven’t used computers as often as others and just the stress of working in the online type of environment is probably hard for people that haven’t done a lot of computer work previously.” (Phase 2)
“I think people’s real fear is that there is going to be a lot of typing and they’re not really good with typing.” (Phase 2)
Positive Comments (Overall Rank = 8th)
Both Phase 1 and Phase 2 participants were able to say positive things about EHRs. Not surprisingly, the Phase 1 participants, given their eligibility to participate in this study had the least number of positive comments out of all the ten themes.
“So if these nurses all love it and they can do it … then, shoot I can do it too.” (Phase 1)
“I’m not against things that are gonna make the job more efficient. If what they bring in means that it’s going to give me more bedside time then I am more than happy to learn it.” (Phase 1)
“The record is comprehensive everybody can share it. It will be available across the [hospital] I think they see advantages of… and the ability for the program to actually cue them for things they wouldn’t remember.” (Phase 2)
“The legibility was a really big thing for them, so there were some other comments. That it made it clearer and safer so that you could actually read it.” (Phase 2)
Generations (Overall Rank = 9th)
This is the first time in recent history that four different generations of nurses work together: the Veterans born between 1922 and 1943, Baby Boomers born between 1943 and 1960, Generation Xers born between 1960 and 1980 and the Nexters born between 1980 and 2000 (Clausing, Kurtz, Prendeville & Walt, 2003). These generations share some common values but they also exhibit differences stemming from the experiences of their eras. Veterans and Boomers remember a world without email or internet, cell phones, and when desk top computers and laptops were luxury items purchased by academics and businesses. The Xers and Nexters choose instant messaging and cell phone video or text messaging over email which they find outdated and too slow (Clausing et. al., 2003). Both Phase 1 and Phase 2 participants mentioned that the generational differences between people may have an impact on EHR implementation.
“I’m not from a generation where there is computers. I didn’t grow up with them. I don’t use them.” (Phase 1)
“You know, because of my age, and where I come from, you know, just the whole electronic world isn’t, isn’t um, easy. It’s not like students that are coming out of school now that it’s [computer use], it’s natural for them. I think for the, the young ones coming in, it will just be like, I don’t think it will be much of anything for them.” (Phase 1)
“I think there’s a few junior girls on the floor that, you know, are a little bit more comfortable, a bit more literate with this [computer use]. But most of us, like I said, this, it just makes no sense at all. (Phase 1)
“I think some of it is age related. Umm, we do have an older workforce, so I think that for them, uhh, they may not have grown up using computers.” (Phase 2)
“I think that there’s a fear of anything electronic – well just a lack of familiarity. Whereas, there is a younger group of nurses that are coming in that are, have spent their lives on computers and internet, so they are very comfortable with it.” (Phase 2)
“A lot of these nurses don’t have computers at home. They aren’t really as computer savvy as perhaps some of the younger nurses coming in. They didn’t grow up with computers. Ummm, so that makes things you know difficult for them to try and wrap there head around all this electronic documentation.” (Phase 2)
Negative Comments (Overall Rank = 10th)
Both Phase 1 and Phase 2 participants had generalized negative comments about EHRs. Not surprisingly, the Phase 2 participants, due to their leadership roles, had the least number of negative comments out of all the ten themes.
“Actually, I told my team that I’ll do all patient care, if they just do all the charting.” (Phase 1)
“I’ll be honest if that’s what it’s [EHR] going to do, I’ll do everything I can to make sure it doesn’t work and that it doesn’t get implemented because that takes away from our very own ability.” (Phase 1)
“I mean, some people say it’s [EHR] great, but I very much doubt if in five years from now, the day before I retire I’d say “Oh yeah, it worked out really well” (laughing).” (Phase 1)
“I don’t think it [EHR implementation] was very thought out, planned out or handled very well.” (Phase 2)
Triangulation Results
In an effort to validate the results arising from the main study participants (Phase 1 participants), the themes and their resulting rank were compared between the two phases of the study. The thematic ranking by percentiles is shown in Table 5. The top four thematic categories, resource needs, change & transition, documentation, and technology, were consistent between both phases (Group A in Table 5). The fifth through seventh themes, nursing roles, diminished caring, and computer literacy, were also the same between phases (Group B in Table 5). Lastly, the final three themes, positive comments, generations, and negative comments, were also similar between phases (Group C in Table 5). The thematic clustering seen in groups A, B, and C adds validity and meaning to the coded themes for both the participants in Phase 1 and by the Phase 2 formal and informal leaders of study participants.
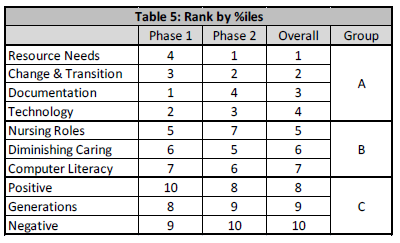
Table 5: Themes Ranked by Percentile
It is interesting to note that the phase 1 participants had the most comments or concerns about documentation and technology. Since all Phase 1 participants documented patient care routinely and would be required to interact with EHR technology daily, it is not surprising that they commented on these concerns more often than Phase 2 participants who might not need to document in patient charts. Conversely, the Phase 2 participants had the most comments about resource needs, change and transition. Many Phase 2 participants were in a position that they had to plan for and fund resource needs as well as deal with larger change management issues in their formal or informal leadership roles. Therefore, the fact that Phase 2 participants commented on concerns about resource needs, change and transition more often than the Phase 1 participants was not unexpected.
Follow-Up and Behavioural Avoidance
All the nurses who participated in Phase 1 interviews consented to be contacted one year after their initial interview to determine their employment status. Of the eleven Phase 1 participants, all nurses remained employed in their same units one year after the original interview. In that one year timeframe, six nurses units’ had implemented EHRs while the other five nurses worked in units that were approximately two months away from EHR implementation. While the nurses stated that they would rather not work in their units during the EHR implementation, there is no evidence to support that their opinions led to actual behavioural changes.
The Theory of Planned Behaviour is a psychological theory which links attitudes to behaviour (Ajzen, 1991). Ajzen stated that an individual’s attitude, norms and perceived behavioural control formed an intention to behave in a certain way. The stronger the intention, the more likely the person was to perform the behaviour. The researchers hypothesized that the nurses may seek to avoid working in their units during the implementation of EHRs, but this was not observed in this study. These nurses may have had strong attitudes, norms and perceived behavioural control, but they may not have had sufficient actual behavioural control to implement their intentions. In fact, one participant, in speaking directly to the younger interviewer, implied that s/he did not have the financial control to retire even though s/he would have liked to do so.
“Save your money! Write that down! Save your money, put it into retirement, and get out sooner.” (Phase 1)
This may explain why, in follow-up, none of the nurses had actually left the profession or moved to another unit.
Discussion
The intended audience for the results of this research include: staff of private or public corporations or health care systems who are involved in the implementation of EHR’s, administrative staff seeking insight into early or unanticipated loss of nursing staff, nurses interested in giving voice to their experiences, and health professionals interested in the path these nurses have travelled. But what to make of it all?
Reports about staff resistance to EHR implementation, previously explored retrospectively, presented methodological drawbacks such as poor recall and loss of key informants (Creswell, 2007). These issues created a critical gap in the literature given that staff resistance to EHR’s can severely impact EHR implementation plans, even leading to the closure of some EHR implementation projects (Scott, Rundall, Vogt, & Hsu, 2003). The current research study addressed this literature gap through qualitative research methods applied prior to EHR implementation.
Understanding the thoughts and opinions and listening to the needs of nurses is essential to support nurses during major transitions such as EHR implementation. Uncovering the path these nurses have taken when agreeing with ‘the statement’ has allowed insight into potential barriers to successful EHR implementation. The findings presented above could be valuable in the planning stage of EHR implementation, facilitating the implementation teams’ awareness of areas of concern. Integrating the identified themes into quantitative measurement indicators for rapid quantitative research could help centers’ preparing for an EHR launch. This research with its qualitatively derived themes and sub themes would allow the creation of an evidenced based validated set of indicators. These indicators could be developed into a straightforward quantitative survey for use prior to EHR implementation. This would allow early identification of hot issues and areas of concern thus allowing for early intervention through education or improved communication strategies.
Lastly, triangulation of the themes between nurses and formal or informal leaders raised an awareness of the overlap between the two groups. In this research, the analysis revealed that the formal or informal leaders had excellent insight into the concerns of these nurses. The reassuring message, that formal leaders are actually aware of nurses’ concerns, is key to communicating with front-line staff.
Conclusion
Establishing an integrated EHR system is a national priority in both Canada and the USA with practical implications for individual nurses, nurse leaders, hospitals and nursing as a profession. Through qualitative research using extreme case sampling, ten major themes were uncovered which expressed the thoughts and opinions of nurses who agreed with a statement that they would rather retire or change jobs than work in their current position during EHR implementation. The themes were validated through triangulation with formal and informal leaders. The ten themes may become a conduit to uncover solutions applicable for improved EHR implementation plans and nurse retention, which may correspondingly result in improved healthcare for patients.
Acknowledgements
We would like to acknowledge the assistance of these 4th year nursing students: Marie Reeves, Leena Ruparelia, Nancy Britnell, Heather Kewageshig, Lindsay Garlough, Stephanie Abu-Jazar, Bianca Salem & Daryl Geerts.
References
Ajzen, I. (1991). The theory of planned behaviour. Organizational Behaviour and Human Decision Processes, 50, 179-211.
Canadian Federation of Nurses Unions (2012), Research to action: Applied workplace solutions for nurses
Clausing, S. L. ,Kurtz, D. l., Prendeville, J., & Walt, J. L. (2003). Generational diversity – the Nexters. American Operating Room Nurses Journal, 78 (3), 373-379.
Creswell, J. W. (2007). Qualitative inquiry & research design choosing among five approaches. (2nd ed.) Thousand Oaks, CA: Sage Publications.
Halcomb, E.J. & Andrew, S. (2005). Triangulation as a method for contemporary nursing research. Nurse Researcher, 13 (2), 71-82.
Kaufman, D., Roberts, W. D., Merrill, J., Lai, T., & Bakken, S. (2006). Applying an evaluation framework for health information system design, development, and implementation. Nursing Research, 55(2), S37-S42.
Lee, T. T. (2007). Nurses’ experiences using a nursing information system: early stage of technology implementation. CIN: Computers, Informatics, Nursing, 25, 294-300.
McLane, S. (2005). Designing an EMR planning process based on staff attitudes toward and opinions about computers in healthcare. CIN: Computers, Informatics, Nursing, 23, 85-92.
Poissant, L., Pereira, J., Tamblyn, R. & Kawasumi, Y. (2005). The impact of electronic health records on time efficiency of physicians and nurses: A systematic review. Journal of the American Medical Informatics Association, 12, 505-516.
Scott, J. T., Rundall, T. G., Vogt, T. M., & Hsu, J. (2003). Kaiser Permanente’s experience of implementing an electronic medical record: A qualitative study. British Medical Journal, 331, 1313-1316.
Stevenson, J.E., Nilsson, G.C., Petersson, G.I. and Johansson, P.E. (2010) Nurses’ experience of using electronic patient records in everyday practice in acute/inpatient ward settings: A literature review. Health Informatics Journal, 16, 63-72.
Canadian Institute for Health Information, Regulated Nurses: Canadian Trends, 2005 to 2009 (Ottawa, Ont.: CIHI, 2010).
Author Bios
Wendy Seidlitz, RN, BScN, MSc, Clinical Informatics Specialist
McMaster Children’s Hospital, Hamilton Health Sciences
Bio: Wendy is a Clinical Informatics Specialist and prior to this was a Clinical Educator and bedside nurse in the NICU. Her interests include data for knowledge translation to achieve improved outcomes; technology as a tool to facilitate improvements; and the impact of electronic health records on nursing.
Dr. Susan Blatz, RN, MEd, PhD, Clinical Nurse Specialist
McMaster Children’s Hospital, Hamilton Health Sciences
Bio: Susan has worked in the NICU as a clinical nurse specialist, clinical educator, transport nurse and as a staff nurse. She is a faculty member at McMaster University School of Nursing. Her role includes research examining clinical nursing issues and practices and evaluating quality of care and patient safety issues.
Barb Jennings, RN, MSHSA, Program Manager
McMaster Children’s Hospital, Hamilton Health Sciences
Bio: Barb has over thirty years experience in pediatrics and critical care and is currently the Pediatric Critical Care manager at McMaster Children’s Hospital and a Nursing Faculty member at McMaster University. She, along with the Pediatric Critical Care team, led the successful pilot of E-documentation for Hamilton Health Sciences.
Rebecca LaRocca, RN, BScN, MSc, Registered Nurse
McMaster Children’s Hospital, Hamilton Health Sciences
Bio: Rebecca holds a Master of Science from McMaster University (2011) and an Honours Bachelor of Science in Nursing from Brock University (2006). She is a bedside nurse in the Pediatric Critical Care Unit at McMaster Children’s Hospital and a Nursing Faculty member at Brock University.







