eHealth: A concept analysis from a nursing perspective
by Jeff Reed, RN BScN
Master of Nursing Student,
Arthur Labatt Family School of Nursing, Western University
Abstract
Aim. This article is a report of a concept analysis of eHealth
Background. eHealth is ubiquitous in Canada’s healthcare system. A great deal of ambiguity exists around the definition of eHealth, especially within nursing, although it involves the implementation of electronic communication or information technology in the context of healthcare. Analysis of eHealth from a nursing perspective is needed to guide education, knowledge development, research, and policy.
Data Sources. A literature search was done using electronic literature databases, websites, internet search engines and the grey literature. Materials from the past two decades were analyzed.
Method. Walker and Avant’s (2011) framework for concept analysis was used to analyze the concept.
Discussion. eHealth can be identified by four attributes: electronic transformation, connectivity, efficiency, and quality of care. Antecedents of eHealth include, but are not limited to clinician readiness, organizational and technical preparation, and patient trust. The consequences of eHealth are unclear and warrant further research, especially within the nursing profession.
Conclusion. This concept analysis clarified some of the ambiguities of eHealth found within the literature and also proposed a definition of eHealth that is unique to nursing.
Keywords: Concept Analysis, eHealth, Nursing
Introduction
Some of the nurses who read this analysis may remember the days when healthcare was solely paper-based and the integration of technology into the healthcare system was far off on the horizon. These nurses may also attest to the speed at which technology has engulfed the way that care has been delivered to individuals, communities and populations over the last two decades into what we have come to know as eHealth (electronic health). The emergence of technology in healthcare has followed a Moore’s Law- like progression where the technology we use is changing and developing exponentially (Wickramasinghe, 2013), making eHealth omnipresent in all facets of the healthcare sector today. This growth has transformed the concept of eHealth from what was originally meant to describe the application of information and communications technology (Health Canada, 2010), to a catch-basin for anything technology-related in healthcare. The pervasiveness of the term has made the development of an operational definition a difficult task, especially for the nursing profession. This is troublesome, given that nurses are at the forefront of this technology revolution and represent the largest regulated health care provider group in Canada (Health Canada, 2013). There is an obvious need for an analysis of this concept to guide policy, research and practice within nursing, and as such, the underlying goal is to clarify the meaning of, and develop an operational definition of eHealth within the realm of nursing practice.
Methods
A review of nursing, medical, information technology studies, business literature, as well as internet grey literature was conducted over the past two decades to the present time. The terms ‘eHealth’, ‘e-health’, and ‘electronic-health’ were used as search keywords to review the literature linked to this concept.
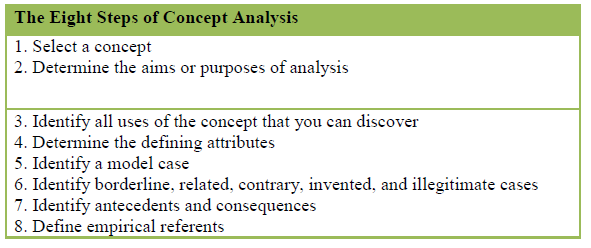
The procedure used for this article was adopted from Walker and Avant’s (2011) classic procedure for concept analysis. This 8 step procedure (Table 1) examines the basic elements of a concept and helps to develop a consistent operational definition that increases the validity of the construct within nursing practice.
Table 1: The Eight Steps of Concept Analysis (adapted from Walker & Avant, 2011)
Findings
History of the Concept
The elements of eHealth in Canada began to form at the end of the 20th century with the advent of the different government advisory groups and committees who strove to develop a strategy to optimize health information sharing and technology. A report from the National Forum on Health (1997) recommended the rapid development of a national health information system. This was reaffirmed by a report of the Advisory Council on Health Infostructure (1999), which highlighted potential benefits of a national health information highway. This impelled a multitude of government funding, programs, and networks to emerge in the early twenty-first century, all with the common goal of advancing the healthcare system with technology (Health Canada, 2010). Around this time, early definitions of eHealth began to emerge that describe this paradigm shift in healthcare. Perhaps the most common definition comes from Eysenbach (2001), who described eHealth as:
an emerging field in the intersection of medical informatics, public health and business, referring to the health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterizes not only a technical development, but also a state-of-mind, a way of thinking, an attitude, and a commitment for networked global thinking, to improve health care locally, regionally, and world-wide by using information and communication technology (e.20).
The biggest investment in Canada’s eHealth strategy was the development of Canada Health Infoway (CHI) in 2001, which acts as a strategic investor of government funding to foster the adoption and use of health information technologies. CHI has supported the growth of a number of eHealth strategies, but the most notable is its pursuit of implementing an interoperable Electronic Health Record (EHR) (CHI, 2013). In this time span, Canada has become internationally recognized for its advancement of eHealth strategies and health systems planning (Information and Communications Technology Council, 2009), but this transformation of the healthcare system has left a common definition of eHealth in the grey.
Uses of the Concept
Searches for eHealth produced no results when using three popular online dictionaries (Merriam Webster Dictionary, 2013; Cambridge Dictionary, 2013; Oxford Dictionary, 2013), demonstrating the infancy of this concept beyond the realm of health and information studies. The McGraw-Hill Concise Dictionary of Modern Medicine defined eHealth as a philosophy that empowers health care consumers with online information and services (as cited in the Farlex online referencing tool, 2013).
Two large systematic reviews of health, informatics, and business literature attempted to surmise a definition of eHealth. Oh, Rizo, Enkin, and Jadad (2005) described the term as an all-encompassing neologism that lacks operational clarity. Of the 51 unique published definitions of eHealth in this review, only health and technology were common themes. Oh et al. (2005) described the aforementioned definition by Eysenbach (2001) as appearing most frequently in the literature. Another commonly cited definition teased out by this review was that of Mitchell (1999) who describes eHealth as a new term to demonstrate the relationship of electronic communication and information technology in the healthcare sector. It is evident from this review that although eHealth has a strong presence in the health literature, researchers need to develop a consistent definition.
Another comprehensive review from Pagliari et al. (2005) examined the eHealth concept based on a wide body of literature across disciplines. This review found 387 publications containing the term eHealth, of which, 77 appeared in clinical journals, 61 in health service journals, 7 in finance-related journals, 3 in journals related to medical education, and 28 in other journals that couldn’t be categorized. They found the most common topics were related to telemedicine, the internet, scope of eHealth, trends in eHealth and challenges with eHealth. Pagliaria et al. (2005) identified 36 unique definitions of eHealth within these publications, each with varying themes and foci, however most definitions cite the use of information and communications technologies (ICTs). In particular, the overwhelming presence of the internet and electronic data in eHealth definitions suggests that the concept may be unique from the more tangible technology addressed in the informatics world.
A review of nursing literature and resources revealed that many researchers referenced eHealth in articles without actually giving a clear definition. Harrison (2006) described e-Health as “an all-encompassing term for the combined use of electronic information and communication technology in the health sector” (p. 284). Peate (2013) defined eHealth as a way to promote health and well being by using the power of information management and communication technology. The e-Health Nurses Network (2007) describe the term as employing technology to enhance professional practice and promote health and wellness. The International Council of Nurses (2013) offers an eHealth Programme aimed at supporting telehealth technologies and connecting nurses worldwide, but the program lacks a clear definition of what eHealth actually is. The Registered Nurses’ Association of Ontario (RNAO) (n.d.) takes a broader approach by defining eHealth as any healthcare practice supported by electronic communication or information and communication technology (ICT). Like other disciplines, the eHealth concept has flooded the nursing literature without any consensus on a clear definition. An existing theme common to the nursing literature was that eHealth is part of a holistic approach to health care and should be used to enhance wellness in clients.
Defining Attributes
The goal of this stage in the concept analysis is to underscore a collection of attributes most frequently associated with the concept and that set it apart from other similar concepts (Walker & Avant, 2011). The following attributes were garnered from a variety of sources related to eHealth and fall on a conceptual continuum that ranges from tangible descriptors to the abstract.
Electronic Transformation
It comes as no surprise that the most common attribute associated with eHealth is the delivery of healthcare in an electronic state. Traditional methods of service delivery, communication, and information sharing have rapidly evolved, escaping the confines of a paper-based system and entering the digital world. Despite the variance in definitions of eHealth, most share the commonality of having the internet and digital ICTs at its core. Wyatt and Liu (2002) claimed that eHealth is characterized by the use of the internet by a variety of stakeholders to access health information, services, and support. Deluca and Enmark (2001) added that eHealth has been branded by the electronic exchange of health information across organizations. Moreover, Broderick and Smaltz (2003) also identified the application of the internet and other related technologies in healthcare as a foundation to eHealth. It is evident that the cornerstone to eHealth across all disciplines is healthcare delivered electronically, albeit in various forms. Kreps and Neuhauser (2010) described eHealth as taking the form of many internet-based platforms such as interactive websites for patients and clinicians, web-portals, e-mail, online communities, and gaming. Some claim that eHealth extends beyond the typical internet applications. For instance, McConnell (2002) states that eHealth could apply to a wide variety of technologies, including “health information systems, databases, genomics, biotechnology, eLearning, continuing professional development, nanotechnology, drug treatment technologies, decision making tools, diagnostic aids, eLibraries, laboratory tools, and robotics” (p.1). The overwhelming presence of electronic healthcare delivery within the eHealth literature is certainly the biggest commonality, but although it gives shape to the eHealth construct, more attributes are needed to distinguish its uniqueness in the nursing world.
Connectivity
The advent of eHealth has undoubtedly made the world of healthcare a smaller place. Consumers, clinicians, administration, organizations and other stakeholders have been able to leverage technology to communicate more efficiently and more effortlessly, and as such, connectivity emerges as a multi-faceted theme within the eHealth construct.
The use or enhancement of services through electronic means is one way in which eHealth demonstrates connectivity. Clinicians and organizations alike have implemented creative ways with which to improve care and promote health across the continuum of care. For instance, a recent study demonstrated a significant increase in knowledge of sexually transmitted infections in youth who were allocated to a text message and email based education intervention (Lim et al., 2012). Another electronic solution, offered by a Canadian hospital, is a patient-centred internet portal called My CARE Source. This portal gives patients within the oncology and renal care programs access to treatment plan information, symptom monitoring, appointment management, personal health profiles, education information, a discussion board, and a clinician directory (DeLenardo, 2004). Programs like these demonstrate that connecting health consumers to programs and services has been made possible with the advent of eHealth.
Connectivity to health care providers using electronic means extends the consumer to clinician relationship from face-to-face interactions into the realm of the digital world. The College of Nurses of Ontario (2009) defined this realm as telepractice, or the delivery and management of health services using technologies like smart phones, faxes, internet, videoconferencing, teleradiology and telerobotics. eHealth communication between patients and providers has the potential to enhance patients’ knowledge, confidence, health care interaction, and health decision-making (Wald, Dube, & Anthony, 2007), and when used effectively, may positively influence client health and well-being (Dutta-Bergman, 2005). These interactions introduce a new degree of connectivity between stakeholders, allowing for communication where it may not have been possible before.
Connectivity also relates to access to information, in that eHealth opens the doors to a great wealth of data for both consumers and clinicians. It is estimated that more than 60% of Canadians use the internet to search for health information (Statistics Canada, 2008), and that nearly 5% of all internet searches worldwide relate to health (Eysenbach & Kohler, 2003). Patients are accessing information to manage their health independently or to help them decide whether or not to seek medical attention, and also to supplement information given to them by health care providers (McMullan, 2006). This profound access to health information allows patients to be more engaged and informed in their care, but is not unique to consumers. Through eHealth technologies, clinicians are also equipped with access to current health literature, information and resources. eHealth can assist nurses in acquiring, maintaining, and advancing their knowledge and skills to enhance care in the moment, or achieve personal and professional goals (RNAO, n.d.), all of which ultimately benefit the client. Great efforts are also being made in Canada to streamline patient information into EHRs, which would contain current and past medical history, progress notes, immunizations, allergies, and demographic information (Garets & Davis, 2006), with the ultimate goal of having an interoperable and interlinked record accessible to organizations and clinicians across a continuum of care. Connectivity related to growing information access demonstrates how eHealth is broadening the scope of knowledge in all healthcare stakeholders.
Efficiency
The potential to improve effectiveness and efficiency in healthcare has been a hallmark of eHealth since its birth. This is another one of its obvious defining attributes, given that any eHealth strategy deemed inefficient would contradict its purpose to improve current practice. This is of particular interest in today’s healthcare arena, where fiscal pressures influence decision-making and healthcare management. One recent study showed that the introduction of an EHR in an inpatient ward reduced unnecessary diagnostic tests, decreased transcription costs, decreased copy-paper costs, and reduced medication errors, ultimately leading to a rapid improvement in costs and client safety (Zlabek, Wickus, & Mathiason, 2011). Although no definitive conclusion exists related to the value for money for health information technologies (O’Reilly, Tarride, Goeree, Lokker, & McKibbon, 2012), they may offer cost advantages while improving care. eHealth strategies may also improve the access to care for different regions and populations. Humphreys (2002) claims that eHealth may be a cost-effective solution to coordinate care and improve the equity of access to health services by patients and professionals in rural communities, demonstrating that eHealth may be part of a solution to address geographical disparities in health.
Quality of Care
eHealth solutions are not just about improving efficiencies in care, enhancing work-flow, and reducing healthcare spending, rather they also provide an opportunity to improve the quality of care. Thede (2003) described how information, coupled with nursing expertise and knowledge, can promote sound clinical decisions. The Royal College of Nursing (2012) pointed out that eHealth has the potential improve patient monitoring among nurses and allows for quicker diagnosis, discussion, and interventions. Furthermore, the increased access to information in nursing may produce better client outcomes. For instance, the implementation of an EHR in the care of those with diabetes yielded an improvement in systolic and diastolic blood pressure, smoking cessation, and other health outcome measures (Herrin et al., 2012). Other motivators for eHealth solutions include enhanced patient safety, reduced errors in healthcare, and the ability to document and quantify improved outcomes (Robles, 2009). It is clear that the merits of eHealth are not limited to cost savings and efficiencies, but also improving healthcare delivery and the quality of care provided to healthcare consumers.
Identifying Cases
Model Case
A model case is an example of the concept that exhibits all of its defining attributes and qualities. Walker and Avant (2011) describe a model case as, “a pure case of the concept, a paradigmatic example, or a pure exemplar” (p.163). The following is a description of an intervention currently being studied that exemplifies eHealth, as well as a fictitious example of two study participants within this study who will demonstrate the attributes of the concept.
The Mental Health Engagement Network (MHEN) is focused on putting technology into the hands of mental health clients and their mental health care providers to demonstrate a more effective and efficient mental health care service delivery model. The intervention involves a customized electronic personal health record application, the Lawson SMART record, and interactive tools that support a novel way to provide clients with standardized health services, ongoing monitoring and regular communication with their mental health care providers. This innovative solution may help to coordinate care across a continuum by ensuring that services are more accessible, patient-centered, and promote the empowerment of individuals. From a population perspective, this proposed system re-design has the potential to reduce or prevent acute episodes of mental illness and reduce the severe constraints on an already over-burdened health care system (Forchuk et al., 2013).
Ryan is a 21 year old male who lives and works outside of London, Ontario, Canada. Four years ago, Ryan experienced an acute psychotic episode while at school and was subsequently admitted to an adolescent psychosis unit in London’s major hospital for just over two weeks. After Ryan was discharged, he was linked up with the hospital’s outpatient psychosis program where he attended regular follow up visits with his psychiatrist, social service visits with the social worker, and occasional group meetings with other mental healthcare consumers. Ryan’s health over the years has been unsteady to say the least. He experienced multiple subsequent admissions to the hospital for psychiatric reasons, he dropped out of high school, citing a lack of interest and motivation, he hasn’t been able to retain employment, and he often misses appointments with the care providers at the program. About six months ago, Anna, a Registered Nurse who often liaises with Ryan in the outpatient program, invited him to be a part of a new and exciting study which uses an electronic personal health record (EPHR) to collaboratively manage health. Ryan agreed to participate in the study, and set up a plan with Anna to use the EPHR for regular electronic communication, mood tracking, medication reminders, appointment scheduling, goal setting, and smoking cessation. Over the last six months, Anna has noticed incredible improvements in Ryan’s attitude, health, and overall quality of life. Ryan has been using the EPHR to consistently update Anna on his life and health, which he finds far easier than finding a ride into London to meet face to face with her at the program. He finds that his electronic medication list not only reminds him when to take his daily medications, but it also reminds him when he needs a prescription refill, something that used to be a major barrier to him. Tracking his mood and symptoms made him recognize that he was experiencing lethargy and fatigue after taking a certain morning medication. After liaising with his psychiatrist, Ryan changed this medication to the evening and has since cited an increase in energy and liveliness throughout the day and better rest at night. Ryan has decided to postpone employment so that he can focus on his studies. He used the goal setting application within the EPHR to design a plan to achieve his high school diploma and is now enrolled in two correspondence classes, which he finds manageable. Finally, Ryan used the tracker within the EPHR to monitor his smoking habits and accessed smoking cessation information online from his mobile device given to him for the study. He has been completely tobacco free for two months. Anna is thrilled with the outcomes from this intervention, and although she devotes more time to keeping up to date with the EPHR, she is confident that she is actually saving time by preventing adverse episodes and promoting Ryan’s health.
This case highlights the potential for electronic health technologies to improve healthcare efficiency, enhance patient outcomes, and maximize the connectivity among healthcare stakeholders and services. Ryan and Anna were able to take full advantage of the ability to share information and connect electronically. Monitoring and tracking his own health information made Ryan more aware of his health and encouraged him to take an active role in health maintenance. He was also able to access information, resources, and services that were either previously unavailable or very difficult to receive because of his lifestyle and geographical location. Apart from the efficiencies in this method of health services delivery, a number of improvements were seen in Ryan’s health. He optimized his symptom management, improved his adherence to his medication routine, he quit smoking, and also began to address some of the social determinants of health in his life. Apart from the healthy outcomes of her client, Anna also cited time savings and prevention as a major benefit to this intervention. Overall, this case exemplifies the pillars of eHealth discussed in the latter steps of this analysis and helps to materialize the construct using a reality-based situation.
Borderline Case
A borderline case has many of the same elements as a model case however one or more of the defining attributes differs in some way. It is closely connected to the case, but has some dissimilarity that makes it inherently distinguishable from the concept being studied (Walker & Avant, 2011). The following is a borderline case to demonstrate the variances in other concepts, albeit small ones, to help differentiate eHealth.
Judy, a 32 year old Nurse Practitioner, has recently taken over a new role and patient caseload in a well-baby outpatient clinic. This clinic serves a population that typically lives below the poverty line and has a high incidence of teen pregnancies. When Judy came into the role, she noticed that there were an unusually high number of missed appointments at the clinic that interfered with patient-flow and on some occasions caused adverse health outcomes for certain clients. Judy decided to implement a strategy where the clinic assistant would make day-of phone calls to patients reminding them of their appointments and offering them two bus tickets if needed. Over the next year, Judy evaluated this strategy based on a number of outcomes. She observed a significant increase in appointment attendance among the teenage mothers, a reduction in adverse events due to missed appointments, and she noticed that she was able to see more patients in a day with less down-time.
The strategy that Judy implemented in this borderline case demonstrates many of the same attributes as the model case. By setting up phone reminders for her patients, Judy enhanced the connectivity to her patients with the ultimate goal of increasing clinic attendance. By increasing the number of patients she saw in a day and by reducing her downtime in between patients, Judy made her clinic-flow more efficient and organized. Furthermore, she observed a reduction in adverse health outcomes that were related to missed appointments. This case exhibits many of the same attributes as the model case described earlier, however, it lacks the electronic robustness and innovation that was seen in the EPHR. Although telephone interventions are not obsolete in the realm of healthcare, they certainly lag behind the technologies that exemplify the eHealth movement today, and for that reason, this case is deemed borderline to the concept of eHealth.
The model case and borderline case presented in this analysis provide enough insight to distinguish the concept of eHealth, and as such, the contrary and related cases were omitted.
Antecedents and Consequences
Walker and Avant (2011) define antecedents as, “events or incidents that must occur or be in place prior to the occurrence of the concept (p.167), which can help elucidate social contexts in which the concept occurs in.
Antecedents
Clinician readiness for change is a commonly cited antecedent to the implementation of eHealth practices. Bozak (2003) demonstrates that nurses have a tendency to question new eHealth technologies used for practice and can be reluctant to change and fear disruption to workflow. This is also met with excitement and enthusiasm from other nurses, demonstrating varying degrees of opinion and attitudes among the nursing cohort. A study that measured nurses’ perceptions of an eHealth overhaul in practice found a number of factors that influenced nurses’ readiness for change. Of these factors, computer self-efficacy was found to be the strongest predictor of readiness for nurses, which suggests that knowledge development is a key factor to transitions in practice and should be a precursor to any eHealth initiative (Turner, 2007). Another study showed the necessary factors to promote eHealth readiness were setting realistic goals and expectations, involving users at all points of the planning process, early buy-in from staff, determining how workflows may change with implementation, and learning from other organizations or clinicians who have already implemented the technologies (Cherry & Owen, 2008). eHealth initiatives may be intimidating and undesirable to some clinicians, thus it is imperative to provide adequate preparation and promotion measures before new technologies can be successfully integrated into practice.
Although clinician readiness is central to practice changes, technical and organizational grounding and preparation are also antecedents to eHealth implementation. Greenhalgh and Russell (2010) suggest that organizations need to be aware of the expectations and constraints within the eHealth strategies and to consider how they may work in real-life situations. One organization that implemented an eHealth strategy for patient care retrospectively recognized that effective and consistent technical support, budgeting for extra staff, and nursing requirements incorporated into system design would have been crucial elements to increase the success of the program (Laurie-Shaw, Taylor, & Roach, 2006).
Patient or client trust is another antecedent for eHealth. eHealth allows personal health information to be shared effectively and efficiently, but it also poses new risks to the privacy and confidentiality of healthcare consumers. With the advent of new technology comes a balance between privacy and the access to all available health information, and in order for eHealth to exist, it is crucial to strike this balance by protecting sensitive data and keeping consumer trust (Patient Trust Key to Health, 2013). Rynning (2007) reaffirmed this notion in suggesting that eHealth strategies like EHRs not only require technical compatibility, but also concern for legal, social, and cultural context related to privacy and confidentiality. This demonstrates that although certain technologies are promising from a clinical and organizational perspective, client well-being and trust needs to be the impetus for eHealth integration into healthcare.
Consequences
Walker and Avant (2011) described consequences as defining outcomes as a result of the concept. These are difficult to identify within the construct of eHealth, given the concept is novel, understudied, and its definition remains largely ambiguous. Furthermore, the variance in eHealth makes it impossible to imply consequential causation, and as such, analysis only allows for the identification of how eHealth may influence healthcare. Some common consequences that eHealth may influence include the promotion of client self-care, health, and communication, the transition of decision making and responsibility from the professional to the consumer, and the expedited provision of information for all stakeholders (Pagliari et al., 2005). The general understanding of eHealth from the literature echoes a sense of optimism and positivity from stakeholders. Definitions and attributes focused on benefits, improvements, and efficiencies as a result of eHealth (Oh et al., 2005), and while some of the literature identified drawbacks of certain technologies, eHealth was never surmised to be a blunder of the healthcare system. While it is nearly impossible to pinpoint a tangible and consistent consequence of eHealth as a concept, it has certainly transformed how all stakeholders react with the healthcare system, express expectations for the future, and shape attitudes toward technology.
Empirical Referents
According to Walker and Avant (2011), “empirical referents are not tools to measure the concept”, but rather “the means by which you can recognize or measure the defining characteristics or attributes” (p.168). Empirical referents provide the clinician with observable phenomena to measure eHealth in the healthcare setting.
The CONSORT-EHEALTH V1.6.1 is a guideline currently being developed that is useful for health research across all disciplines. This instrument uses a number of eHealth items and sub-items to guide reports of web-based and mobile interventions in healthcare. These guidelines will enhance the quality of research and maintain consistency of eHealth reports, which can facilitate systematic reviews, knowledge translation, and understanding (Eysenbach, 2011).
Atkinson (2007) also developed an empirical referent for eHealth designed to help eHealth developers to improve the adoption of their applications. Factor analysis demonstrated that relative advantage, simplicity, trialability, observability, and translatability were able to predict nearly half of the variance in adoption potential. This instrument may help to successfully implement eHealth strategies through all stages of development.
Discussion
This analysis was done to explore the concept of eHealth within our healthcare system, with the ultimate goal of clarifying the meaning and definition of eHealth, reducing ambiguities, and promote consistency in using the concept in practice, research, and everyday life. Walker and Avant’s (2011) framework for analyzing a concept was relatively easy to follow, but perhaps was too simple for the scope and breadth of this concept. The literature review of the concept was so ambiguous that validating attributes and antecedents of eHealth proved to be difficult. It was also a challenge to synthesize consequences of this concept, given its relative age and indistinctiveness within health research.
In spite of the challenges faced in the process, this analysis has contributed to nursing in several ways. One aim of this analysis was to clarify the concept and develop some consistencies in eHealth descriptors, to benefit nurses, consumers, policy makers and other clinicians who have little to no background in eHealth and are faced with a advancing technological healthcare system. It is clear from the literature that there is a great deal of variance in the eHealth concept, making it difficult to abridge. This analysis has identified and related attributes within all disciplinary research that illustrate the concept of eHealth, such as the electronic transformation of current practices, the connectivity of consumers, clinicians and other stakeholders to information and each other, efficiency among workflow and clinical processes, and improved quality of care of those who are served. These attributes will certainly help to identify what eHealth is and is not for future reference in clinical practice, decision-making, and research.
Furthermore, this analysis identifies antecedents to eHealth that cannot be ignored during this time of rapid change and eHealth implementation. Decision-makers must consider the readiness of clinicians, organizational and technical preparation, and patient trust when developing and implementing eHealth strategies in order to ensure the smooth rollout of new service delivery models. Consequences of this concept were difficult to identify since this concept is in its infancy and the literature is far from conclusive. Even though no tangible consequences can be identified with certainty, eHealth is expected to enhance the same health outcomes we expect from current practice. This comes as no surprise, since eHealth is not meant to overhaul the current system, but rather improve clinical processes by interacting harmoniously with current practices (Shabot, 2004). The clarity of attributes, antecedents, and consequences within this analysis may help to educate stakeholders at all levels, and may be useful in research and knowledge development, decision-making, and even strategy development.
The second aim of the analysis was to develop an operational definition of eHealth unique to nursing that may be referenced in a number of settings by stakeholders at all levels. Based on the findings and critical reflection, the following definition was developed:
“eHealth is not merely the application of electronic communication and information technology in healthcare. The simple fact that it is developed by and used for humans suggests that it is inherently sociological. It reflects the collective societal attitudes, lifestyles, and determinants of health in which it is found and therefore will develop and be evaluated in a context that is in constant flux. As such, eHealth within the realm of nursing needs to be a balance between its technical and social elements, with the ultimate goal of having a holistic approach to care with the patient at its core.”
Conclusions
Using Walker and Avant’s (2011) eight steps for concept analysis, both a clear understanding of and concise definition of eHealth were identified. After deliberation of the growing body of literature, unique attributes and antecedents were identified that will be useful for future knowledge development, research, education and decision-making. A clear definition of eHealth also gives a unique nursing perspective to eHealth that adds to its understanding and conceptualization.
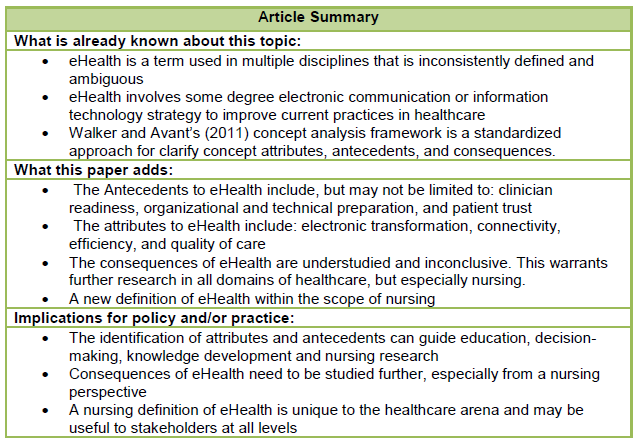
Table 2: Summary of Article Findings
References
Advisory Council on Health Infostructure. (1999). Canada health infoway: Paths to better health. Canada’s Health Infostructure. Retrieved from: http://www.hc-sc.gc.ca
Atkinson, N.L. (2007). Developing a questionnaire to measure perceived attributes of eHealth innovations. American Journal of Health Behaviour, 31(6), 612-621. doi:10.55555/ajhb.2007.31.6.612
Bozak, M., (2003). Using Lewin’s Force Field Analysis in implementing nursing information system. Computers in Nursing, 21(2), 80-85. Retrieved from: http://journals.lww.com/cinjournal
Broderick, M., & Smaltz, D. (2003). HIMSS E-Health white paper: e-Health defined.Chicago: Healthcare Information and Management Systems Society. Retrieved from: http://www.himss.org/content/files/ehealth_whitepaper.pdf.
Canada Health Infoway. (2013). Transforming health care in Canada through information technology. About Infoway. Retrieved from: https://www.infoway-inforoute.ca
Cherry, B., & Owen, D. (2008). Determining factors of organizational readiness for technology adoption in Ling-Term Care facilities. TTUHSC LTC Technology Readiness Project: A Final Report. Retrieved from: https://www.dads.texas.gov
College of Nurses of Ontario. (2009). Telepractice. Retrieved from: http://www.cno.org/docs/prac/41041_telephone.pdf
DeLenardo, C. (2004). Grand River Hospital’s internet-based solutions empower patient managed care. Healthcare Quarterly, 7(3), 110-111. Retrieved from: http://www.longwoods.com/website/jobsite/HQ7.3GRH.pdf
Deluca, J. M., Enmark, R. (2001). The latest revolution. What solutions will technology offer? Health Forum Journal, 44(1), 22-25. Retrieved from: http:// ncbi.nlm.nih.gov
Dutta-Bergman, M.J. (2005). The relation between health-orientation, provider-patient communication, and satisfaction: An individual-difference approach. Health Communication, 18(3), 291-303. doi:10.1207/s15327027hc1803_6
eHealth. (n.d.). In Cambridge Dictionaries Online, Retrieved from: http://dictionary.cambridge.org/
eHealth. (n.d.). In Merriam Webster Online, Retrieved from: http://www.merriam-webster.com/dictionary/eHealth
eHealth. (n.d.). In Oxford Dictionaries Online, Retrieved from: http://www.oxforddictionaries.com/
eHealth (2013). In Farlex Online Dictionary, Retrieved from: http://www.thefreedictionary.com/
E-Health Nurses Network. (2007). What is e-Health? Retrieved from: http://www.ehealthnurses.org.uk/index.html
Eysenbach, G. (2001). What is eHealth? Journal of Medical Internet Research, 3(2), e20. doi:10.2196/jmir.3.2.e20
Eysenbach, G. (2011). CONSORT-EHEALTH: Improving and standardizing evaluation reports of web-based and mobile health interventions. Journal of Medical Internet Research, 13(4), e126. doi:10.2196/jmir.1923
Eysenbach, G., & Kohler, C. (2003). What is the prevalence of health-related searches on the World Wide Web? Qualitative and quantitative analysis of search engine queries on the internet. AMIA Annual Symposium Proceedings, 225-229. Retrieved from: http://www.amia.org
Forchuk, C., Rudnick, A., Hoch, J., Donelle, L., Reiss, J.,… McKillop, M. (2013). Mental health engagement network (MHEN). International Journal on Advances in Life Sciences, 5(1&2), 1-10. Retrieved from: http://www.thinkmind.org
Garets, D., & Davis, M. (2006). Electronic medical records vs. electronic health records: Yes, there is a difference. A HIMSS Analytics White Paper. Retrieved from: http://www.himssanalytics.org/docs/WP_EMR_EHR.pdf
Greenhalgh, T., & Russell, J. (2010). Why do evaluations of eHealth programs fail? An alternative set of guiding principles. PLoS Medicine, 7(11), 1-5. doi: 10.1371/journal.pmed.1000360
Harrison, J.P. (2006). The role of E-Health in the changing health care environment. Nursing Economics , 24(6), 283-288. Retrieved from: https://www.nursingeconomics.net
Health Canada. (2010). eHealth. The Healthcare System. Retrieved from: http://www.hc-sc.gc.ca
Health Canada. (2013). Nursing issues: General Statistics. The Healthcare System. Retrieved from: http://www.hc-sc.gc.ca
Herrin, J., da Graca, B., Nicewander, D., Fullerton, C., Aponte, P., Stanek, G., & … Ballard, D. (2012). The effectiveness of implementing an electronic health record on diabetes care and outcomes. Health Services Research, 47(4), 1522-1540. doi:10.1111/j.1475-6773.2011.01370.x
Humphreys, J. (2002). Health service models in rural and remote Australia. In: Wilkinson D, Blue, I, (eds.) The New Rural Health. South Melbourne: Oxford University Press, 273-296.
Information and Communications Technology Council. (2009). eHealth in Canada: Current trends and future challenges. Retrieved from: http://www.ictc-ctic.ca
International Council of Nurses. (2013). EHEALTH. Pillars & Programmes. Retrieved from: http://www.icn.ch/pillarsprograms/ehealth/
Kreps, G.L., & Neuhauser, L. (2010). New directions in eHealth communication: Opportunities and challenges. Patient Education and Counseling, 78, 329-336. doi:10.1016/j.pec.2010.01.013
Laurie-Shaw, B., Taylor, W., & Roach, C. (2006). Focus on clinical best practices, patient safety and operational efficiency. Healthcare Quarterly, 10(special issue), 50-56. Retrieved from: http://www.longwoods.com
Lim, M.S.C., Hocking, J. S., Aitken, C. K., Fairley, C. K., Jordan, L., Lewis, J. A., & Hellard, M. E. (2012). Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. Journal of Epidemiology & Community Health, 66(1), 69-74. doi:10.1136/jech.2009.100396
McConnell, H. (2002). eHealth international. eHealth International, 1(1), 1-2. doi:10.1186/1476-3591-1-1
McMullen, M. (2006). Patients using the internet to obtain health information: how this affects the patient-health professional relationship. Patient Education and Counseling, 63(1-2), 24-28. doi:10.1016/j.pec.2005.10.006
Mitchell, J. (1999). From telehealth to e-health: The unstoppable rise of e-health. Canberra,
Australia: Commonwealth Department of Communications, Information Technology and the Arts (DOCITA).
National Forum on Health. (1997). Canada health action: Building on the legacy. The Final report of the National Forum on Health. Retrieved from: http://www.hc-sc.gc.ca
Oh, H., Rizo, C., Enkin, M., & Jadad, A. (2005). What is eHealth (3): A systematic review of published definitions. Journal of Medical Internet Research, 7(1), e1. doi:10.2196/jmir.7.1.e1
O’Reilly, D., Tarride, J., Goeree, R., Lokker, C., & McKibbon, K. (2012). The economics of health information technology in medication management: a systematic review of economic evaluations. Journal of The American Medical Informatics Association, 19(3), 423-438. doi:10.1136/amiajnl-2011-000310
Patient trust key to eHealth. (2013). Australian Nursing & Midwifery Journal, 21(3), 18. Retrieved from: http://www.anmf.org.au/pages/anmj?
Peate, I. (2013). Technology, health and the home: eHealth and the community nurse. British Journal Of Community Nursing, 18(5), 222-227. Retrieved from: www.bjcn.co.uk/?
Pagliari, C., Sloan, D., Gregor, P., Sullivan, F., Detmer, D., Kahan, J.P., … & MacGillivray, S. (2005). What is eHealth (4): A scoping exercise to map the field. Journal of Medical Internet Research, 7(1), e9. doi: 10.2197/jmir.7.1.e9
Registered Nurses’ Association of Ontario. (N.D.). eHealth defined. In Nursing and eHealth Course Education Course. Retrieved from: http://elearning.rnao.ca/#ehealth
Robles, J. (2009). The effect of the electronic medical record on nurses’ work. Creative Nursing, 15(1), 31-35. doi: 10.1891/1078-4535.15.1.31
Royal College of Nursing. (2012). Using technology for people with long term conditions: Guidance for nurse practitioners. RCN: London. Retrieved from: http://www.rcn.org.uk
Rynning, E. (2007). Public trust and privacy in shared electronic health records. European Journal of Health Law, 14, 105-112. doi:10.1163/092902707X211668
Shabot, M., (2004). Ten commandments for implementing clinical information systems. Baylor University Medical Center Proceedings, 17, 265-269. Retrieved from: http://www.baylorhealth.edu/proceedings/?
Statistics Canada. (2008). Getting a second opinion: Health information and the internet. Statistics Canada, Health Reports. Retrieved from: http://www.statcan.gc.ca
Thede, L. (2003). Informatics and Nursing: Opportunities & Challenges (2nd Ed). New York: Lippincott Williams & Wilkins
Turner, D. (2007). Clinician readiness for transition to a fully integrated electronic health care delivery system. (Doctoral dissertation). Retrieved from: http:// gradworks.umi.com
Wald, H.S., Dube, C.E., Anthony, D.C. (2007). Untangling the web – the impact of internet use on health care and the physician-patient relationship. Patient Education and Counseling, 68, 218-224. Retrieved from: http://www.pec-journal.com
Walker, L., & Avant, K. (2011). Strategies for theory construction in nursing (5th ed.) New York: Prentice Hall
Wickramasinghe, N. (2013). The possibilities are only limited by our imaginations. In R. Bali, I. Troshani, S. Goldberg & N. Wickramasinghe (Eds.), Pervasive Health Knowledge Management (pp. 243-244). doi:doi:10.1007/978-1-4614-4514-2_18
Wyatt, J.C., Liu, J.L.Y. (2002). Basic concepts in medical informatics. Journal of Epidemiology and Community Health, 56(11), 808-812. doi: 10.1136/jech.56.11.808
Zlabek, J., Wickus, J., & Mathiason, M. (2011). Early cost and safety benefits of an inpatient electronic health record. Journal of the American Medical Informatics Association, 18(2), 169-172. doi:10.1136/jamia.2010.007229.
Biographical Statement
Mr. Reed is currently working towards his Master of Nursing Degree at Western University in London, Ontario Canada. His research interests include optimizing technology and information systems to support nursing practice and to provide quality care to clients.







