Understanding Gap Analyses of Clinical Information System Requirements
by Steve Iduye BN, MHI
Faculty of Computer Science
Dalhousie University
Halifax, NS, Canada
Abstract
This paper draws an inference from a conventional approach that compares client system requirements with another successful CIS platform to bridge the gaps for a system upgrade. It also extrapolates on the inevitability of using the ISO/IEC 25010:2011 framework in designing an evidence-based gap analysis for clinical information system requirement transformation projects. In the conventional approach, the client’s requirements are categorized as functional, non-functional, external interface, user-requirements, or business requirements for comparison against another client with similar requirements in its CIS platform.
In the quality model framework (ISO/IEC 25010:2011), criteria are used as a benchmark to measure the degree of gaps in the requirements for any CIS platform that requires an upgrade. The conventional approach may or may not provide upgraded features based on the CIS to which the client requirements were compared. In the quality model framework approach, the criteria are scientifically tested and approved for the CIS requirement deployment by a software engineering standard organization (ISO).
Keywords: CIS; ISO/IEC 25010:2011; EHR; Digital Health; Evidenced-Based.
Introduction
In the ongoing debate on what constitutes the right requirements for clinical information system (CIS) replacement, enhancement and integration (i.e., transformation) is moving from paper-based information management systems to electronic medical records. Meeting the needs of clients is critical for any CIS transformation project to succeed. Moreover, the transition of clinical information from paper-based to electronic records requires a gap analysis that uses benchmark assessment tools and standard guidelines are needed to achieve evidence-based solutions to reach the client’s goals and objective. In this paper, an evidence-based CIS requirement gap analysis is undertaken to shed light on where the health institution’s CIS stands now and where it intends to be in the future.
A CIS is frequently described as the interactions between individuals, processes, and technology to support fundamental information operations, management, and availability, for the sake of improving healthcare services (Almunawar & Anshari, 2011). CIS requirements should always be geared towards improving the safety of clinical data and its reliability in a consistent and accurate manner. Different requirements proposed by CIS end-users or clients are based on the clinical workflow that clients intend to capture or improve. Irrespective of the main CIS transformation objectives, it should not take away from the primary objective for designing a CIS, which is to help clinicians manage their patients’ care seamlessly. The requirements for clinical information workflow require both clinical and technical details to show their interrelationship or interdependence, with a detailed description of CIS components that are needed for system developers to optimize the entire system configuration. Because of the complicated and detailed description of the components, the design of hospital information systems is changing from data-collection or storage platform to an interactive, interoperable and a secured platform. Health informaticians must understand how the EHR specifications and requirements are designed and built with the profound methodology mentioned above. This understanding will prevent building redundant functionalities or using functions that do not help clinicians do their job proficiently.
Methods and Results
Healthcare systems generate large amounts of clinical data that can come in different forms. The data may be stored in several databases with different management platforms (Jardim, 2013). Because of the complexity of the data structures or storage requirements, constant overhauls or transformations are needed to meet the patients’ needs. As health institutions are embracing the implementation of electronic health records or pursuing CIS upgrades, health informaticians will play an unprecedented role in current and future trends. For clinical system analysts, CIS requirements need to be elicited, expressed, prioritized, analyzed, and managed in collaboration with the clients or end-users to achieve a good result. Imminent danger awaits a project implementation when the processes are carried out with little or no contribution from the clients.
Depending on the chosen methodology, the processes should be sequential and followed by the analyst. To fulfill the requirements, nurse informaticians need to engage the end-users and clients through a series of investigative and interactive processes to identify and differentiate their needs from their wants. Open-ended questions must probe and clarify the details of the client’s requirements. This differs from requirement gathering, because of the absence of face-to-face or constant interactions between the development team and the clients. With regards to the requirements, nurse informaticians need to use visual or textual representations of the user stories (i.e., storyboards) and use cases that are tailored to the project so that the team members can have a better understanding of the process. To prioritize the requirements, clients must specify a list of their needs from “must have” requirements, to “should have” requirements, to “could have” requirements, while considering the time, budget, and other constraints. The list of requirements must be constantly checked for clarity and consistency to uncover what might be missing, over-stated, or understated: this process is called the requirements analysis. One of the key activities is the managing of requirements, which is focused on keeping track on what is elicited, expressed, prioritized, analyzed, or changed as the project moves forward.
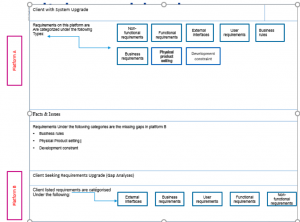
Conventional Approach
Two scenarios are presented in this paper to illustrate how the gap analysis of CIS requirements can be done. Clients often look for solution upgrades that will likely improve the clinical and technical infrastructure of their CIS platform. In the first scenario, a client requests a gap analysis of their requirements after a series of discussions with the system analyst. The following list represents a summary of client’s present CIS status and requirements:
- The CIS design and architecture are not scalable or cost-effective
- The system is effective but not interactive or user-friendly
- The client’s CIS needs to be transformed to be a user-oriented, updated version of the desired technical and clinical solution
- The clinical data needs to be interoperable and integrated and the documents need to be upgraded
- The business intelligence platform needs to be optimized for hospital service utilization
By using a simple conventional method, the client’s requirements are categorized as functional, non-functional, external interface, user-requirements, or business requirements. These categories are further compared with another client with similar requirements and some upgrades to their CIS platform. The conventional approach focuses on comparing the system requirements of the two CIS solutions and finding those features that the client with the upgraded version has but the client requesting the gap analysis does not have.
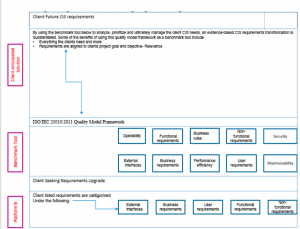
ISO/IEC 25010:2011 Quality Framework
In scenario two, the ISO/IEC 25010:2011 quality model becomes a benchmark tool for measuring the degree of gaps in the requirements for any CIS platform that requires an upgrade. It also provides a road map for any institution desiring future CIS requirement upgrades or a transformation in its EHR projects. The two fundamental principles for the framework include:
The ISO/IEC 25010:2011 quality model provides features that translate the outcome of interactions when the features are used; it also has metrics that measure the extent to which a product meets the needs of specified users in a specified context of use (Idri, Bachiri, & Fernández-Alemán, 2016).
The ISO/IEC 25010:2011 software quality model also consists of eight unique characteristics that include the following:
- Functional suitability: Does the product provide features that meet the needs under certain conditions?
- Reliability: Does the system perform certain functions under specified conditions for a duration of time?
- Performance efficiency: Is the performance equal to the level of resources used under certain conditions?
- Operability: Does the product have features that allow it to be understood correctly or learned, and is it user-friendly, when used in certain conditions?
- Does the system have security for data protection that prevents unauthorized third-party access?
- Does the system have features that promote interoperability or other interfaces?
- Maintainability: Can modifications be made?
- Transferability: Is the system transferable from one hardware, software, or another operational system or environment to another? (ISO/IEC-25010, 2011)
The implication of this approach is to provide information about the difference between the two solutions and offer recommendations for navigating through the changes required for a system upgrade or transformation. This gap analysis will help in ranking the system requirements, and by comparing the system requirements with the ISO best practices, and the level of importance for each requirement will be known by the client and the development team. Consequently, the client will gain insight about the possible areas for improvement. Although clients know what they want, best practices can help to inform them about why their needs should be changed.
Discussion
In regards to CIS requirements and digital health transformation projects, Obeidat (2016) indicated a problem with identifying the precise client requirements throughout the entire engagement, stemming from human or workplace complexities. Because of human error, and the omission or commission in the entire requirements, the result could be a poor design by the development team. The evidence-based gap analysis of the requirements plays a significant role in EHR procurement and implementation as all of the requirement details are essential for building an interactive design. The conventional approach has a limitation in that it minimizes the time while meeting the needs of the client, but this methodology does not measure the degree of gaps, or provide a benchmark tool for comparison with applicable standards and best practices. Moreover, a simple comparison of the system requirements for platform A and B, and implementing the upgraded features for platform A, can make platform B redundant if the client needs a change in the future. On the other hand, the quality model framework can be time consuming and expensive, because it involves many details that need to be translated for the client’s needs.
The success of a software implementation project, like any other project, is determined by the workplace complexities such as budget, time, and project scope. Digital health projects require informaticians to participate in every aspect of the project, from requirement elicitation, the analysis of system requirements, finding the gaps in present and future requirements, and engaging stakeholders, to performing the implementation to prevent a mismatch between the client’s requirements and the final deliverables or expectations. To facilitate the process of change conforming to the client’s expectations, Chopra (2011) argued that rather than modeling requirements as being critical or noncritical, the requirements should be modeled for the context in which they are relevant. To achieve a state of completeness in system design, an evidence-based gap analysis of the requirements should meet the client’s needs at every stage of system development and at the final deliverable stage. The relevance of system requirements is best defined by understanding the client’s project goals and objectives. A gap analysis that is entrenched in applicable standard practices can provide the means to an end by mitigating any chance of error in managing the requirements or in implementing a poorly designed solution.
Conclusion
This paper considers two different methodologies that have been found useful in a gap analysis for system requirements. The first method uses a simple comparison of requirements. The client’s present requirements are compared to any EHR platform that the client and the system analyst considers a success. The differences in the requirements between the two platforms are considered for the client’s system upgrade. The second method illustrates the use of gap analysis with the ISO/IEC 25010:2011 quality model as a benchmark tool to drive the current CIS requirements to reach the desired state.
Besides discussing the relationships between current and future CIS requirements, this paper points out the relevance of requirement elicitation, expression, prioritizing, analyses, and requirement management to capture the client’s correct needs. As requirement activities become more elaborate in workflow mapping, clinical informaticians or clinical system analysts will continue playing a vital role in system requirement gathering, analyses, testing, and implementation. Moreover, the roles of clinical application management consultants will also continue playing a significant role in helping clinicians navigate from the current state of CIS to the future expectations using a best practice methodology.
Conflict of Interest
None
References
Almunawar, M. N., & Anshari, M. (2011). Health information systems (HIS): Concept and technology. In Proceedings of the International Conference on Informatics for Development, 2011.
Chopra, A. K. (2011). Requirements-driven adaptation: Compliance, context, uncertainty, and systems. Requirements@Run. 2nd International Workshop, pp. 32-36.
ISO/IEC 25010.2011. (2011). Systems and software engineering – Systems and software quality requirements and evaluation (SQuaRE) – System and software quality models. Retrieved from https://www.iso.org/standard/35733.html
Idri, A., Bachiri, M., & Fernández-Alemán, J. L. (2016). A framework for evaluating the software product quality of pregnancy monitoring mobile personal health records. Journal of Medical Systems, 40: 50.
Jardim, S. V. B. (2013). The electronic health record and its contribution to healthcare information systems interoperability. Procedia Technology, 9, 940-948.
Obeidat, R. (2016). Managing requirement changes in health informatics projects. International Management Review. 12(1), 39-51.