Impact of Hospital Information Systems on patient care: Nurses’ perceptions
INTERNATIONAL ARTICLE
by Hesamaddin Kamalzadeh Takhti, MBA, PhD Student
Dr. Azizah Abdul Rahman
Samireh Abedini, MSN, PhD Studemt
Sedigheh Abedini, MS-MCH, PhD Student
Abstract
Aim: To explore the perceptions of nurses about the use of a Hospital Information System (HIS) in the provision of patient care in terms of information and system quality.
Background: Although HIS are becoming a vital part of nursing care, it is unclear what system characteristics contribute to nursing acceptance.
Method: A cross-sectional survey research design was applied to collect data from nurses in the sample.
Results: The survey response rate was 82 per cent (140 out of 170 nurses responded) and the resultant Cronbach’s alpha statistic was 0.78. Generally, 87.9 per cent of respondents utilized HIS in their daily practice. System characteristics identified by the nurses as beneficial included timeliness, reliability, data completeness and accuracy of information.
Conclusion: The findings of this study indicated that the nurses in this sample perceived that HIS qualities of timeliness and reliability contributed to complete and accurate information about patients in nursing practice. These qualities appeared to enhance the value of the HIS in the nurses’ perception.
Keywords: Patient care; Nursing care; Information quality; System quality, Perceptions, Hospital Information Systems.
Introduction
The rapid introduction of Information Systems (IS) in all aspects of society has left little time to consider the impacts or develop policies to take maximum advantage of these systems. Most organizations, including hospitals either use or are planning to implement IS in some capacity. The progressive growth of Information Technology (IT) has led hospital administrators to recognize IT as a powerful tool to enhance their organization’s productivity (James, Parag, & David, 1996). Many hospitals around the world are in the process of moving away from paper-based health information and implementing electronic health information to support patient care.
This shift appears to be timely. The sheer volume and variety of health information has caused problems in the delivery of patient care when using traditional information systems. For example, paper-based medical records are easily misplaced and can cause serious problems, such as the need for repeated diagnostic tests, delays in the planning of care, legal complications, and delayed patient discharges. Hence, hospitals have started to use Hospital Information System (HIS) to facilitate and improve the process of patient care via the generation of electronic health records (Ting-Ting, 2004).
HIS are designed to support clinicians in accessing and working with a variety of patient information (Gruber, Cummings, Leblanc, & Smith, 2009) and promoting health care quality through coordinated information sharing (Beuscart-Ze´phir, Anceaux, Crinquette, & Renard, 2001). HIS were first introduced in the 1980s to store more generic information such as data from laboratory examinations (Shusaku, 2002). The main goal of current HIS is to manage information from all healthcare-related activities, including planning, monitoring, coordination, and decision making. Key objectives of HIS implementation are to improve the availability of patient records by making information accessible for patient care; to decrease the wait time for diagnostic information, such as laboratory results; and to improve patient administration procedures (Kobus, Peter, Jakes, Mark, & Jeremy, 1999).
HIS implementation seems essential to meet increasing healthcare demands and the associated diagnostic, treatment and administrative system burdens; to support better patient care planning, and clinical or administrative decision making (Edward, 1995). The real-time access, exchange and receipt of clinical data provided by HIS have improved clinical documentation, reduced the duplication of care services, and supported better decision making related to patient care (Tiina, Tarja, Paula, Marianne, & Ilmari, 2009).
Nurses are the key providers of patient care, including assessment, diagnosis and intervention (T. Lee, 2004). Nurses must quickly incorporate information about various patients and immediately organize and interpret the information to plan quality care (Bosman, 2009). Thus, it is imperative that HIS are designed to meet nursing care requirements to optimally coordinate patient care activities (S. Lee & Mcelmurry, 2010).
Patient Care
The concept of patient care can be defined as the creation of more value for patients through the removal of all non-value-added steps or actions (Victoria & Kannan, 2008). The current administrative emphasis on the management of frequently used resources, cost control, the effectiveness of patient care, and improved quality and responsibility, reinforces the importance of optimal patient care. An important precondition of optimal patient care is that patient information is completely and accurately recorded and accessible (Ammenwerth, et al., 2001). Undoubtedly, if a patient’s medical records are used as a means of communication between health care providers; these records will function as unique tools for planning, coordinating and organizing patient care (Nilmini & Steve, 2008). Time required for patient care is related to complete, timely and adequate patient medical information. Optimal patient care requires accurate real-time data acquisition and updated patient profiles (Masoud & Ric, 2008). To investigate the effects of a particular HIS on the delivery of patient care, we asked the question, “What information and system characteristics of HIS support nurses in the patient care process?”
The importance of information and system quality
Since the advent of HIS development, many high-level managers and health care planners have strived to detect factors that influence the quality of patient care. Many believe that the quality of health care is enhanced through information collected and accessed via HIS. Information and HIS quality are linked with the support of effective, timely and appropriate care services, reduction of health risk; efficiently streamlining clinical and administrative tasks such as communicating with patients, their families and other healthcare professionals; monitoring patient awareness; and achieving strategic planning and community health management goals.
However, information alone is not valuable; its value is derived from the changes that it influences in decision making, so information quality is defined as data that are fit for use by data consumers (Richard & Diane, 1996). Health care environments are increasingly dependent on information and the volume of the data collected, stored and used has greatly increased, while computer dependence has also increased. Health care information and related data have grown larger and faster in the past decade. This information is more operational and complex than previous information. However, larger and more complex data are not necessarily better data. The most important issue in this field is the use of high-quality information to improve patient care. Thus, health information can be most effective when the data is high in quality.
A model of information system success provided by DeLone and McLean (2003) showed that information quality and system quality affect organizational services. Researchers have indicated that information quality consists of particular attributes, such as completeness, accuracy and relevance (Haslina & Sharifah, 2005; William & Ephraim, 2003) . System quality in patient care measures important HIS characteristics such as timeliness and reliability.
Timeliness refers to the length of time taken for information to be delivered to users, in other words, the period of the time between sending an order and the order being executed (Van Der, Tange, Troost, & Hasman, 2003). However, timely information depends on the nature of the information, as information sensitivity is different in various segments. Reliability means that repeated processes of collecting, storing and presenting data show similar results. Repeated tests on the same data must generate the same results. Hence, reliability is considered to be the cornerstone of information value (Yong, Huadeng, & Xiliang, 2009).
Methodology
This research study was conducted using a descriptive cross-sectional design to examine nurses’ perceptions of the impact of an HIS on the provision of patient care. The population sample for the study included nurses from a 960-bed hospital. This study used a systematic random sampling procedure to select the participants. The majority of respondents were female (99.3 per cent). Three quarters (73.6 per cent) of the respondents had more than 3 years of nursing experience. Data was collected using a five-point Likert scale questionnaire. The five-point Likert rating scale (1=Strongly Disagree, 2=Disagree, 3=Neutral, 4=Agree, 5=Strongly Agree) allowed individuals to rate their perceptions of the questions with answers that were readily converted to numbers. SPSS software was used to analyze the numerical data that resulted.
Results
The survey response rate was 82 per cent (140 out of 170 nurses responded). Reliability is an important measurement attribute to support consistency of findings over time under the same conditions. Chronbach’s Alpha is the best statistical test for evaluating the reliability of internal consistency. The reliability of the internal consistency of the study’s survey questions tested for a Chronbach’s Alpha of 0.780, which scored higher than the base acceptable level of 0.70 (Kijsanayotina, Pannarunothai, & Speedie, 2009). There was an acceptable internal correlation among the questions and the admissibility of the questions was confirmed.
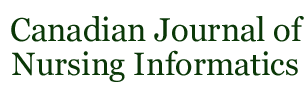
The majority of the respondents showed positive perceptions about HIS implementation in their daily practice (87.9%). In this survey, descriptive statistics were applied to the independent attribute variables (timeliness, reliability, completeness, relevancy) and the dependent variable, patient care. The results are shown in Table 1.
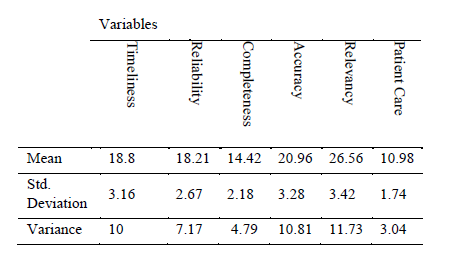
Table 1: Summary of descriptive statistics of variables (N=140)
An analysis of Spearman’s correlation coefficients was performed to measure the relationship between the independent attribute and dependent variables (Table 2).
Table 2: Correlation between independent and dependent variables (N=140)
The analysis suggested some significant relationships. The Spearman’s correlation coefficients of 0.191 for the timeliness of system, 0.210 for reliability of system, 0.316 for completeness of information and 0.174 for accuracy of information were significant at the p< 0.05 level, indicating a positive relationship between the nurses’ perceptions of timeliness and reliability of system, accuracy and completeness of information and quality of patient care. The Spearman’s correlation coefficient of 0.155 for information relevancy with a p-value of 0.67 did not show substantial correlation between this variable and patient care.
Discussion
The purpose of this cross-sectional survey was to explore the perceptions of nurses about the use of a HIS in the provision of patient care in regards to information and system quality. The nurses described their perceptions of HIS and patient care by focusing on questions related to HIS information and system quality. Nurses represent the largest group of healthcare providers across the globe (Aein, Heravi Karimooi, Ahmadi, & Tootoonchi, 2006) and dominant the provision of patient care (Lee, 2004) in the hospital. The perceptions of nurses is an important consideration for measuring perceived value of HIS within the hospital setting.
To date, the most important issue in successful implementation of IT is the acceptance and use of technology by the end users (Boonchai, Supasit & Stuart 2009). Our results show, that an HIS is used daily by nurses (87.9 per cent) in the workplace. Findings suggest that the nurses widely accepted the use of an HIS as a necessary component of their daily practice in the provision of patient care (Lammintakanena, Sarantoa, & Kivinenb, 2010). Nurses use HIS and other electronic information systems for documenting assessments and patient status data (Adams, 1998). HIS systems play an important role in the documentation of nursing care activities.
The results from this descriptive study seem to support key findings reported in the literature. The first precondition of quality patient care is accurate and accessible information. In a digital hospital, HIS provide a electronic health record that becomes a repository for collected data and information related to patient care (Häyrinena, Lammintakanenb, & Sarantob, 2010). Of course, patient care information is available in paper-based systems, but the quality and quantity of the information is often quite low in comparison (Cornelia, et al., 2007). This fact often spurs nurses to become competent in using HIS to document their activities and identify HIS as powerful tools to achieve more complete and accurate information for better patient care. The study results highlighted that information quality in terms of accuracy and completeness proved to be a significant predictor of information usage in the patient care process. So quality of information should be an organizational audit priority in terms of improving nursing performance and patient care (Paul, Anna, June, & Eileen, 2004).
Certain system attributes such as timeliness and reliability are correlated with system use in the delivery of good patient care. Real-time access, exchange and receipt of clinical data reduce the duplication of care services and improved the quality of patient care. For example, some studies suggest that use of computer-based systems create the opportunity for nurses to reduce charting times as well as nursing overtime (Allen & Davis, 1992 ) and increaseg time to carry out patient care (Fraenkel, Cowie, & Daley, 2003). Daily requirement time for all activities involved in manually recording patient data such as vital sign, laboratory results and order prescription are reportedly reduced by utilizing HIS. This leaves more time to spend in providing nursing care – a significant factor that increases the quality of nurses’ practice and improves patient care. Although HIS provide relevant patient information for nursing care (Häyrinena, et al., 2010), the relevancy of information was a less significant predictor in this study. It could be due to the fact that health care information is fluid and subject to change. Therefore, the relationship between what is documented in a HIS and the request for information should be fully developed within the system to provide the right requested information to nurses as they require it.
Conclusion
It is important to understand the potential influence that an information system application can have on nurses’ daily practices. The findings of this study indicate that the quality of an HIS, including attributes such as timeliness and reliability provide complete and accurate information about patients for nursing practice. It seems that an HIS helped administrators and nurses to identify and eliminate ineffective activities involved in the patient process and supported nurses’ daily practice by providing complete, essential data to support optimal patient care.
References
Abele, D., Vincenzo, G., Simona, P., Paola, C., Tiziana, P., Benedetto, M., et al. (2008). The impact of a clinical information system in an intensive care unit. Journal of Clinical Monitoring and Computing 22(1), 31-36.
Adams, J. M. (1998). Health information systems: improving nursing care and cutting costs. MedSurg Nursing, 7(5), 308-309.
Aein, F., Heravi Karimooi, M., Ahmadi, F., & Tootoonchi, M. (2006). Baccalaureate Nursing Curriculum: Its Adjustment with Burden of Diseases as “Disability Adjusted Life Years” in Iran. Journal of Medical Education, 6(2), 7-14.
Al-Ahmadi, H. (2009). Factors affecting performance of hospital nurses in Riyadh Region, Saudi Arabia. International Journal of Health Care Quality Assuranc, 22 (1), 40-54.
Allen, D., & Davis, M. (1992 ). A computerized CIS enhances bedside intensive care. Journal of excellence in nursing leadership, 23(7), 112I,112J,112N,112P.
Ammenwerth, E., Kutscha, U., Kutscha, A., Mahler, C., Eichstadter, R., & Haux, R. (2001). Nursing process documentation systems in clinical routine–prerequisites and experiences. International Journal of Medical Informatics, 64(2), 187 – 200.
Beuscart-Ze´phir, M. C., Anceaux, F., Crinquette, V., & Renard, J. M. (2001). Integrating users’ activity modeling in the design and assessment of hospital electronic patient records: the example of anesthesia. International Journal of Medical Informatics 64(3), 157-171.
Boonchai.K, Supasit.P, & Stuart.M.S. (2009). Factors in?uencing health information technology adoption in Thailand’s community health centers:Applying the UTAUT model. international journal of medical informatics 78, 404-416.
Bosman, R. J. (2009). Impact of computerized information systems on workload in operating room and intensive care unit Best Practice & Research Clinical Anaesthesiology, 23(1), 15-26.
Cornelia, M., Elske, A., Andreas, W., Angelika, T., Torsten, H., Bettina, H., et al. (2007). Effects of a Computer-based Nursing Documentation System on the Quality of Nursing Documentation. Journal of Medical Systems, 31(4), 274-282.
Edward, E. H. (1995). The computer-based patient record vision contrasted with HIS/MIS. International Journal of Bio-Medical Computing, 39, 19-23.
Fraenkel, D., Cowie, M., & Daley, p. (2003). Quality benefits of an intensive care clinical information system. Critical Care Medicine, 31 (1), 120-125.
Gruber, D., Cummings, G. G., Leblanc, L., & Smith, D. L. (2009). Factors Influencing Outcomes of Clinical Information Systems Implementation:A Systematic Review. Computers, Informatics, Nursing 27(3), 151-163.
Haslina, M., & Sharifah, M. S. M. (2005). Acceptance Model of Electronic Medical Record. Journal of Advancing Information and Management Studies, 2(1), 75-92.
Häyrinena, K., Lammintakanenb, J., & Sarantob, K. (2010). Evaluation of electronic nursing documentation—Nursing process model and standardized terminologies as keys to visible and transparent nursing. International journal of medical informatics 79 (1), 554-564.
James, A. R., Parag, C. P., & David, J. P. (1996). End-user perceptions of quality and information technology in health care. Journal of High Technology Management Research, 7(2), 133-147.
Kijsanayotina, B., Pannarunothai, S., & Speedie, S. M. (2009). Factors in?uencing health information technology adoption in Thailand’s community health centers:Applying the UTAUT model. international journal of medical informatics 78, 404-416.
Kobus, H., Peter, L., Jakes, R., Mark, C., & Jeremy, C. W. (1999). Evaluating computerized health information system: Hardware, Software and Human ware: Expriences from the northern province south Africa. Journal of Public Health Medicine, 21(3), 305-310.
Lammintakanena, J., Sarantoa, K., & Kivinenb, T. (2010). Use of electronic information systems in nursing management. International journal of medical informatics, 79 (1), 324-331.
Lee, S., & Mcelmurry, B. (2010). Capturing Nursing Care Workflow Disruptions:Comparison Between Nursing and Physician Workflows. Computers, Informatics, Nursing 28(3), 151-159.
Lee, T. (2004). Evaluation of Computerized Nursing Care Plan:Instrument Development. Journal of Professional Nursing, 20(4), 230-238.
Masoud, M., & Ric, J. (Eds.). (2008) Healthcare Information Systems (Vols. 2). United States of America: Information Science Reference.
Michaei, M. W., & William, R. H. (1996). The Accuracy of Medication Data in an Outpatient Electronic Medical Record. Journal of the American Medical Informatics Association 3(3), 234-244.
Mohan, J. (2004). The Impact of Completeness and Web Use Motivation on the Credibility of e-Health Information. Journal of Communication, 54(2), 253-269.
Nilmini, W., & Steve, G. (Eds.). (2008) Healthcare Information Systems (Vols. 1). United States of America: Information Science Reference.
Paul, B., Anna, S., June, B., & Eileen, B. (2004). The feasibility and potential of organisational peer review audit in community nursing: an example of record keeping. Quality in Primary Care, 12 (2), 109 – 117.
Richard, Y. W., & Diane, M. S. (1996). Beyond Accuracy: What Data Quality Means to Data Consumers. Management Information Systems, 12(4), 5-34.
Shusaku, T. (2002). Medicine Handbook of data mining and knowledge discovery (pp. 798-807): Oxford University Press, Inc.
Tiina, M., Tarja, S., Paula, A., Marianne, M., & Ilmari, R. (2009). The outcomes of regional healthcare information systems in health care: A review of the research literature. International journal of medical informatics, 78(11), 757.
Ting-Ting, L. (2004). Evaluation of Computerized Nursing Care Plan:Instrument Development. Journal of Professional Nursing, 20(4), 230-238.
Van Der, M. J., Tange, H. J., Troost, J., & Hasman, A. (2003). Determinants of Success of Inpatient Clinical Information Systems: A Literature Review. Journal of the American Medical Informatics Association, 10(3), 235-243.
Victoria, H., & Kannan, S. (Eds.). (2008) Healthcare Information Systems (Vols. 1). United States of America: Information Science Reference.
William, H. D., & Ephraim, R. M. (2003). The DeLone and McLean Model of Information Systems Success: A Ten-Year Update. Management Information Systems 19(4), 9-30.
Yong, W., Huadeng, W., & Xiliang, T. (2009). On the Reliability of Information. Paper presented at the Control and Decision Conference.
Author Bios
Hesamaddin Kamalzadeh Takhti, MBA
Master of Business Administration (Information Technology Management)
Faculty of Computer Science & Information Systems, Universiti Teknologi Malaysia
Mailing address: A-7-3, Desa Saujana Apartment, Tmn SG Besi Indah, Seri Kenbengan, Selangor, Malaysia, Post code 43300
HP No: 0060178795363
Email Address: Hesamadin@gmail.com
Dr. Azizah Abdul Rahman
Assoc. Professor
Faculty of Computer Science & Information Systems, Universiti Teknologi Malaysia 81310, Skudai, Johor, Malaysia.
Email Address: azizahra@utm.my
Tel: 607- 5532403
Samireh Abedini, MSN, PhD Studemt
Faculty of Education, Universiti Teknologi Malaysia And Faculty member of Hormozgan university of medical sciences
Mailing address: A-7-3, Desa Saujana Apartment, Tmn SG Besi Indah, Seri Kenbengan, Selangor, Malaysia, Post code 43300
HP No: 006017871 3691
Email Address: Samireha@gmail.com
Sedigheh Abedini, MS-MCH, PhD Student
Faculty member of Hormozgan University of medical sciences
Mailing address: A-7-3, Desa Saujana Apartment, Tmn SG Besi Indah, Seri Kenbengan, Selangor, Malaysia, Post code 43300
HP No: 00989177614328
Email Address: Sabedini45@gmail.com
Editor Reviewers:
Carol McKenney
Wendy Seidlitz
Paulette Lacroix
Editor: June Kaminski