Transforming Nursing Practice: A Model for Digital Health Project Management
by Cynthia Di Tomasso, RN, BScN, Project Manager
MN Student
Athabasca University
Citation: Di Tomasso, C. (2025). Transforming nursing practice: A model for digital health project management. Canadian Journal of Nursing Informatics, 20(3). https://cjni.net/journal/?p=15313

Abstract
This paper presents a comprehensive exploration of nursing theories and their application to contemporary nursing practice, culminating in the development of the Digital Nurse Project Manager Model. The model was developed to integrate holistic assessments and relationship-building to support digital health initiatives, emphasizing the importance of human connection in mitigating uncertainty and resistance among stakeholders. The foundational concepts of nursing—person, environment, health, and nursing—are examined through the lens of personal experiences and theoretical frameworks, highlighting their relevance in delivering patient-centered care. Additionally, the integration of scientific, personal, aesthetic, and ethical knowledge is discussed, underscoring the multifaceted nature of nursing practice.
The paper advocates for active involvement of clinicians in organizational change processes. The development of the Digital Nurse Project Manager Model aims to improve health outcomes and support the evolving healthcare landscape by fostering resilience and adaptability. The conclusion emphasizes the importance of continuous professional development, interdisciplinary collaboration, and the promotion of evidence-based practices to advance the nursing profession and create a healthy environment for the nursing community.
Background
For years, nursing has been rated as one of the most respected and trusted professions across North America (Walker, 2025). This high regard is well-deserved, as nurses consistently demonstrate unwavering dedication, compassion, and expertise in their care for patients. I have seen first-hand the profound impact that nurses can have on individuals and, through their practice, on themselves.
Over time, the meaning of being a nurse has evolved for me. Initially, it was a career path that promised opportunities to travel to places I had admired growing up. Soon, I realized that the profession’s unique commitment and emotional demands were areas where I truly thrived.
It is not the hard skills that I have mastered and the knowledge that was required for and saturated my practice, but it was the conversations and the deep connections that I remember most. The comfort in a client’s eyes or tears shared with family—these moments filled my soul and are at the center of my nursing practice. The foundational concepts of nursing and the knowledge required to understand the profession are multifaceted. Nursing knowledge encompasses scientific, personal, aesthetic, and ethical dimensions, each contributing to a holistic approach that defines the profession. These values, beliefs, and knowledge guide the assessment, planning, implementation, and evaluation of care (Murphy et al., 2010), where nurses provide care that is not only clinically effective but also deeply transformative, addressing the unique needs of each patient (Younas and Quennall, 2019; Bender, 2018).
To fully appreciate the nursing profession, it is important to recognize that its reach extends far beyond traditional care. In a rapidly evolving landscape, nurses are required to lead and participate in digital health initiatives to not only support and influence change but also to safeguard the core values of nursing (International Council of Nurses, 2023). Reflecting on my practice as a project manager, I foster resilience during digital transformation by adopting a holistic approach to relationship building. This approach enables me to promote the highest quality of care, ensuring that healthcare teams and patients receive comprehensive and effective support. This paper examines the values and knowledge that underpin my philosophy of nursing and presents the Digital Nurse Project Manager Model, designed to empower nurses to take on pivotal roles in a rapidly evolving digital healthcare landscape.
Foundational Concepts
Foundational to my philosophy of nursing is the metaparadigm of nursing. In 1984, Fawcett outlined the metaparadigm as four central concepts in nursing—person, environment, health, and nursing—that serve as the framework for understanding the profession (Bender, 2018).
The concept of person refers to the individual receiving care, including their physical, emotional, social, and spiritual dimensions (Fawcett, 1984). At the centerpiece of nursing practice (Kim, 2015), the person concept emphasizes the importance of viewing patients holistically and recognizing their unique needs and experiences. The environment encompasses all external factors that affect the person, including physical surroundings, social conditions, and cultural influences. It highlights the role of the nurse in creating a supportive and healing environment for patients. Health is defined as the overall well-being of the person, encompassing physical, mental, and social aspects. It is not merely the absence of disease but a state of complete physical, mental, and social well-being (Fawcett, 1984). These four concepts form the foundation of nursing practice and guide nurses in delivering holistic, patient-centered care. By understanding and integrating these concepts, nurses can better meet the needs of their patients and contribute to the overall health and well-being of the community (Bender, 2018).
As I reflect on my time at the bedside and the deep emotional connections I have made with patients and families, these four concepts have become much more than theoretical ideas. Bender (2018) offered another reconceptualization of the nursing metaparadigm that aligns with my personal experiences in nursing—where it is not just the application of predefined theories or concepts that define care, but rather the relationships between the nurse, patient, and their environment that emerge in the moment. In these moments, true care becomes apparent; the interconnectedness between the person, their environment, and health becomes clear in the act of caring (Bender, 2018).
Nursing Knowledge
My philosophy of nursing is shaped not only by its core concepts but also by the integration of specialized knowledge (Murphy et al., 2010; Thorne, 2020). Understanding what it means to be a nurse involves recognizing the profound impact of compassion, empathy, and dedication in patient care. These principles guide meaningful interactions and decisions in every aspect of the profession. To effectively embody these principles, nurses must rely on a robust framework of nursing knowledge (Rafii et al., 2021).
Nursing knowledge encompasses scientific, personal, aesthetic, and ethical dimensions, each contributing to the holistic approach that defines the profession. By integrating these diverse forms of knowledge, nurses can provide care that is not only clinically effective but also deeply transformative, addressing the unique needs of each patient (Booth et al., 2021). This multifaceted knowledge is a vital component of nursing, deeply influenced by epistemology—the study of knowledge. Understanding epistemology helps nurses acquire, validate, and apply various types of knowledge, leading to improved patient outcomes and advancements in nursing research and education (Rafii et al., 2021). This comprehensive understanding ensures that nursing practice remains grounded in core disciplinary values and prevents the distortion of nursing knowledge (Thorne, 2020).
Scientific Knowledge
Scientific knowledge, derived from empirical research and measurable observations, forms the scientific basis of nursing practice and is essential for evidence-based practice. Early nursing theorists and model builders were highly influenced by science (Murphy et al., 2010). However, scientific knowledge alone is not sufficient to address the complexities of patient care (Welch, 2020).
Personal Knowledge
Personal and relational knowledge, which emphasizes self-awareness, emotional engagement, and understanding interpersonal relationships, are also relevant to knowing in nursing. These aspects are crucial for forming authentic connections with patients and providing care that is truly patient-centered (Thorne, 2020).
Aesthetic Knowledge
Aesthetic knowledge involves creativity and empathy, allowing nurses to understand and respond to patients’ feelings in a profound way. This type of knowledge transforms nursing from a clinical practice into an art, enabling nurses to address the deeper meaning of situations and foster a holistic approach to care. By seeing beyond immediate clinical symptoms, nurses can understand the broader context of a patient’s life and provide care that addresses emotional and psychological aspects as well (Lindell & Chinn, 2022).
Ethical Knowledge
Ethical knowledge is integral to nursing as a human service profession. It guides nurses to provide care that is clinically competent, inclusive, and compassionate. Ethical knowledge ensures that nurses uphold principles such as justice, autonomy, beneficence, and non-maleficence in their practice. This framework helps nurses make complex decisions that balance the needs and rights of patients with the demands of the healthcare system (Malloy and Fisheim, 2024; Canadian Nurses Association, 2025).
The integration of scientific, personal, relational, aesthetic, and ethical knowledge is crucial for maintaining the integrity of nursing as a discipline. This holistic approach enables nurses to tailor care to each patient’s unique needs and adapt to the complexities of an evolving healthcare system. By combining scientific rigour with personal insight, aesthetic sensitivity, and ethical commitment, nurses can provide care that is not only effective but also deeply compassionate and responsive to the needs of patients.
Application to Practice
Technology in healthcare is advancing rapidly, with nursing playing a crucial role in these shifts. Digital health technologies, such as electronic health records, telehealth, and wearable devices, facilitate a more integrated approach to patient care and aim to improve patient outcomes (International Council of Nurses, 2023). To address the challenges in digital health implementation, it is important to consider the impact on service delivery and health outcomes (Mumtaz et al., 2023). Advocating for nursing involvement ensures that digital health technology is developed and applied in a way that meets the needs of patients, families, communities, and healthcare professionals (International Council of Nurses, 2023).
My exploration of nursing theories has contributed to a solid understanding of the importance of caring and the unique wonders of the profession. However, I am drawn to organizational change theories and guiding principles in the application to my practice, supporting digital modernization projects. Models such as Kotter’s 8-Step Model and Lewin’s 3-Stage Model of Change (Harrison et al., 2021) are examples that have been frequently utilized in healthcare organizational change. More importantly, active involvement of clinicians in the change process has proved essential for achieving and maintaining successful outcomes. Projects that thrived were frequently spearheaded by clinicians or framed around the advantages for patients and staff (Harrison et al., 2021). Previous attempts have been made to conceptualize technology as part of the nursing metaparadigm (Johnson and Carrington, 2023; Bayuo et al., 2023), in that technology plays a crucial role as it intersects and integrates with the established metaparadigm domains (Bayuo et al., 2023).
Digital Nurse Project Manager
Human connection and relationship building are central to my role as a change management lead in a digital modernization project. My primary responsibility is to mitigate uncertainty and resistance among stakeholders, including patients and healthcare professionals. I believe that people can adapt and transform when faced with new challenges. Therefore, I approach assessment with a holistic view, aiming to develop supportive relationships with healthcare teams, fostering resilience and adaptability, ultimately enhancing their ability to provide quality care. The importance of holistic assessment and integration, along with the value of managing organizational change, cannot be overstated. When identifying the impact of change on nurses and patients, a holistic perspective encourages healthcare professionals to consider how new technologies affect not just the clinical aspects of care, but also the emotional, social, and environmental dimensions of patient well-being (International Council of Nurses, 2023).
The Digital Nurse Project Manager Model, which I developed, is introduced in Figure 1 and illustrates the significant impact of my role. This model not only showcases my contributions but also reflects my nursing philosophy, which underscores the importance of utilizing holistic assessments in building relationships to support change adoption and improve health outcomes. Central to my practice is an understanding of the nurse-patient connection, where nursing values and knowledge intersect with a patient’s social determinants of health. The environment surrounding the patient and nurse includes the external factors that can impact the nurse-patient interaction, such as the healthcare setting (Fawcett, 1984). Digital transformation is where the digital nurse project manager exists, outside of but contributing to the nurse and patient in their environment. Shown by three arrows entering the nurse and patient domains, the impact of a change initiative can influence working practices, workflows, and potential outcomes (Harrison et al., 2021). By applying principles of digital transformation, a digital nurse project manager can mitigate this impact. Through effective leadership, active engagement, and supportive activities (for example, training and resources), they can enhance the implementation and adoption of change (Phillips and Klein, 2023; Errida and Lotfi, 2021).
Figure 1
The Digital Nurse Project Manager Model
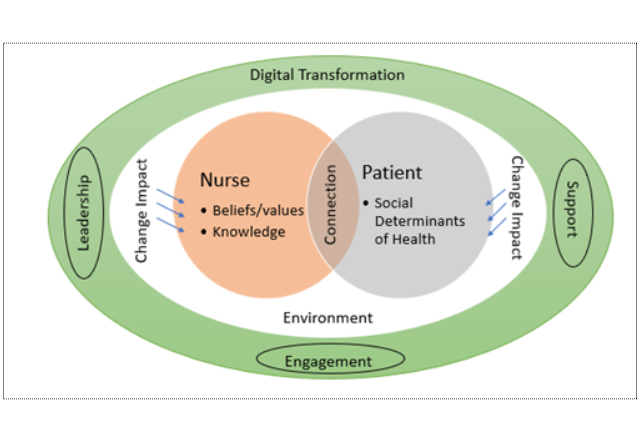
Note: The Digital Health Project Manager Model illustrates the significant impact of holistic change assessments and the application of digital transformation principles in enhancing nurse-patient relationships, supporting change adoption, and improving health outcomes.
References
Bayuo J. (2024). Revisiting the philosophy of technology and nursing: Time to move beyond romancing resistance or resisting romance. Nursing Philosophy. 25(4), e12503. https://doi.org/10.1111/nup.12503
Bender, M. (2018). Re?conceptualizing the nursing metaparadigm: Articulating the philosophical ontology of the nursing discipline that orients inquiry and practice. Nursing Inquiry, 25(3), 1-9. https://escholarship.org/content/qt7tb3224c/qt7tb3224c.pdf
Booth, R. G., Strudwick, G., McBride, S., O’Connor, S., & Solano López, A. L. (2021). How the nursing profession should adapt for a digital future. British Medical Journal. 373, n1190. https://doi.org/10.1136/bmj.n1190
Canadian Nurses Association (2025). The code of ethics for nurses. https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics
Errida, A., Lotfi, B. The determinants of organizational change management success: Literature review and case study. International Journal of Engineering Business Management. 2021;13. https://doi.org/10.1177/18479790211016273
Fawcett, J. (1984). The metaparadigm of nursing: Present status and future refinements. Journal of Nursing Scholars, 16(3), 84-9. https://doi.org/10.1111/j.1547-5069.1984.tb01393.x
Harrison, R., Fischer S., Walpola, R., Chauhan, A., Temitope, B., Mears, S., Le-Dao, H. (2021). Where do models for change management, improvement and implementation meet? A systematic review of the applications of change management models in healthcare. Journal of Healthcare Leadership, 12(13), 85-108. https://doi.org/10.2147/JHL.S289176
International Council of Nurses. (2023). Digital health transformation and nursing practice. Position statement. https://www.icn.ch/sites/default/files/2023-08/ICN%20Position%20Statement%20Digital%20Health%20FINAL%2030.06_EN.pdf
Johnson, E., Carrington, J. M. (2023) Revisiting the nursing metaparadigm: Acknowledging technology as foundational to progressing nursing knowledge. Nursing Inquiry, 30(1), e12502. https://doi.org/10.1111/nin.12502
Kim, H.S. (2015). Nursing knowledge [e-book] (Chapter 6). In The essence of nursing practice: Philosophy and perspective. (pp. 91-99). Springer.
Lindell, D., & Chinn, P. (2022). Nursology: Aesthetic knowing. https://nursology.net/patterns-ofknowing-in-nursing/aesthetic-knowing/
Malloy, D. C., Fisheim, F. (2014). Patient first: Ethics and ontology of nursing care. Annals of Nursing and Practice, 1(3), 1-3. https://www.repository.cam.ac.uk/handle/1810/277110
Mumtaz, H., Riaz, M. H., Wajid, H., Saqib, M., Zeeshan M. H., Khan S. E., Chauhan Y. R., Sohail, H., Vohra, L. I. (2023). Current challenges and potential solutions to the use of digital health technologies in evidence generation: a narrative review. Frontiers in Digital Health, (5). https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2023.1203945
Murphy, F., Williams, A., Pridmore, J. A. (2010). Nursing models and contemporary nursing 1: Their development, uses and limitations. Nursing Times; 106: 23.
Phillips, J., & Klein, J. D. (2023), Change management: From theory to practice. Technology Trends, 67(1):189-197. https://doi.org/10.1007/s11528-022-00775-0
Rafii F, Nasrabadi A. N, Tehrani F. J. (2021). How nurses apply patterns of knowing in clinical practice: A grounded theory study. Ethiopian Journal of Health Sciences, 31(1), 139-146. https://doi.org/10.4314/ejhs.v31i1.16
Thorne, S. (2020). Rethinking Carper’s personal knowing for 21st century nursing. Nursing Philosophy, 21(4), e12307. https://doi.org/10.1111/nup.12307
Walker, A. (2025). Nursing ranked as the most ethical and honest profession for 23rd Year in a Row. Nurse.org https://nurse.org/articles/nursing-ranked-most-honest-profession/
Welch, S. (2020). Caring and esthetics: An argument for a nursing ontology and epistemology. International Journal for Human Caring, 24(3). DOI: 10.20467/HumanCaring-D-19-00062
Younas, A., Quennell, S. (2019). Usefulness of nursing theory?guided practice: An integrative review. Scandinavian Journal of Caring Sciences, 33 (3), 540-555. https://doi.org/10.1111/scs.12670
About the Author
Cynthia Di Tomasso, is a dedicated nursing professional with extensive experience in clinical practice and digital health project management. Currently pursuing a Master of Nursing, Cynthia is committed to advancing nursing practice through interdisciplinary collaboration, evidence-based practices, and innovative digital health solutions.






