The effect of a Competency-based educational application on the knowledge and skills of working with Ventilators in Nursing Students: A randomized controlled trial
by Hadis Ghasemimilsefid, MSc in Intensive Care Nursing
Mostafa Javadi, PhD in Nursing
Khadijeh Nasiriani, PhD in Nursing
Research Centre for Nursing and Midwifery Care, Non-communicable Diseases Research Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Citation: Ghasemimilsefid, H., Javadi, M., & Nasiriani, K. (2025). The effect of a competency-based educational application on the knowledge and skills of working with ventilators in nursing students: A randomized controlled trial. Canadian Journal of Nursing Informatics, 20(1). https://cjni.net/journal/?p=14279

Abstract
The correct use of mechanical ventilation can reduce the length of hospitalization of patients, their mortality and treatment costs. However, it seems that many students do not receive enough training during their studies regarding the use of ventilators, thus, it is necessary to develop and use new educational methods.This study was conducted with the aim of investigating the effect of using a competency-based educational application on the knowledge and skill of working with ventilators with nursing students, and the results showed that their knowledge and skill scores were higher using this method compared to the lecture method.
Background
Patients with acute respiratory failure requiring mechanical ventilation often receive care in intensive care units (ICU). This life-saving measure is one of the most commonly used medical therapies provided in hospital settings (Urner et al, 2018).
Mechanical ventilation refers to the use of a device to replace or assist spontaneous breathing. Invasive mechanical ventilation is a medical procedure that uses an endotracheal tube inserted through the mouth or nose to facilitate the delivery of air into the trachea. This allows for air exchange and supports oxygenation of the lungs. This technique is used in cases of critical illness or respiratory failure when spontaneous breathing is insufficient to maintain normal oxygen levels (Windisch et al., 2018).
There are a variety of indications for mechanical ventilation, generally categorized as either anatomical loss or loss of protective airway mechanisms. Anatomical loss is typically driven by conditions such as edema, injury, burns, infection, and others, while loss of protective mechanisms is usually the result of neurological damage or impairment (intoxicants, brain injury, stroke, and inability to ventilate) (Clemons & Kearns, 2016). Mechanical ventilation is a necessary and commonly used treatment for critically ill adults in intensive care units, and it is also utilized in long-term and subacute patient care.
The main purpose of mechanical ventilation is to normalize arterial blood gas levels and acid-base imbalances by providing adequate ventilation and oxygenation. By unloading respiratory muscles and providing synchronized breathing support, mechanical ventilation can also reduce a patient’s breathing work. In addition, mechanical ventilation can provide long-term respiratory support for patients with chronic ventilatory difficulties (Grossbach et al., 2011). Despite mechanical ventilation being a lifesaving intervention, it comes with the potential for various complications. These include: alveolar damage, airway injury, pneumothorax, oxygen toxicity, and decreased cardiac output (Windisch et al., 2018).
Critical care nurses need specialized skills and knowledge to deal effectively with critical and life and death situations. High-level cognitive and emotional capabilities are essential for navigating the technical and interpersonal challenges encountered daily in such environments. In particular, one of the essential competencies required for critical care nurses is competence in providing effective care to patients on mechanical ventilation support (Mohamed et al., 2019). By providing comprehensive care while also reducing healthcare costs, nurses must possess the knowledge, skills, and abilities to effectively manage patients on mechanical ventilation. It is crucial that educators, students, and nurse practitioners promote a comprehensive approach to learning, with the goal of developing the necessary knowledge and expertise to effectively manage mechanically ventilated patients. Proper ventilation education for all members of the healthcare team will have a significant impact on improving the quality of patient care in this field (Reynolds et al., 2018).
A study conducted in 2018 revealed that senior nursing students lacked proficiency when working with ventilators. ICU nurses often require assistance from other staff to interpret ventilator data (Reynolds et al., 2018). This can jeopardize patient safety, as there could be prolonged exposure to inadequate or unsuitable ventilation. These risks can be life-threatening to patients because they may be exposed to inadequate or inappropriate ventilation for a long time (Radmard et al., 2021). The nurse is frequently the “first-line manager”, responsible for managing patient and ventilator issues. Therefore, it is important that nurses have a thorough understanding of the basics of ventilator support, including the various modes, settings, and alarms. In addition, effective nursing skills in promptly identifying and handling common patient and ventilation problems will allow for optimal care delivery and prevent adverse outcomes. Prompt identification of issues and swift intervention by the nurse can prevent respiratory distress, dyspnea, and increased breathiness and reduce the work needed for ventilation (Grossbach et al., 2011). Nurses providing care to patients who are on ventilators must possess the necessary competence to provide quality nursing care. An effective education program for nursing staff, covering relevant aspects and challenges of managing ventilator patients, will help increase the quality of care (Mohamed et al., 2019).
Currently, books and pamphlets remain important references for ventilator training (Radmard et al., 2021). Textbooks and reference materials can be heavy to carry into classroom and clinical settings. These reference guides are also rapidly outdated, and nursing students need to stay abreast of current clinical practices and guidelines to provide optimal care (George & DeCristofaro, 2016). Additionally, short-term retraining courses are being implemented at hospitals, as the issue is a top priority. However, the face-to-face in-class training method for ventilation has been observed to have a number of limitations. These include overworked nurses, rotating shifts, and high costs leading to poor attendance in classes. Additionally, teaching materials usually remain available only during the class and are difficult to access later. Traditional teaching methods may not consistently meet the evolving needs of instructors and students, and these needs of instructors and learners continuously shape the field of instructional development.
As a result, asynchronous learning techniques have gained popularity in recent years. Asynchronous education prioritizes the learner in the educational process, allowing for independent interaction between instructors and learners irrespective of place and time. Research has demonstrated that nurses need to utilize a variety of educational strategies, including asynchronous activities, to ensure proper education in ventilator management. The use of technology can be an effective solution to provide sufficient training to nurses (Radmard et al., 2021). Mobile smartphones have become an essential tool for healthcare professionals to access clinical resources. This makes them more up to date than traditional print resources. Thus, it is important to provide mobile-friendly resources to professionals to support their best possible practice (George & DeCristofaro, 2016).
The contemporary smartphone has become a powerful tool that facilitates seamless connectivity to a vast repository of information and a wide range of social connections. Smartphones impact almost every aspect of people’s lives as they can be used to connect with friends and family via traditional phone calls and social media platforms like Facebook and Zoom. In addition, smartphones have become an instrumental business tool, enabling the management of emails, calendars, and reference and data management tools for professionals in the healthcare industry (Wyatt & Krauskopf, 2012). Most nursing students are under the age of 30, and they possess advanced familiarity with smartphones and their various functions. The use of smartphones in the clinical educational setting can provide real-time communication with instructors and preceptors, allowing for a faster exchange of information. Additionally, smartphones can support safe care through access to online resources, including videos, podcasts, practice guidelines, and pharmacology information (Phillippi & Wyatt, 2011).
Mobile technology should be more thoroughly incorporated into classroom and laboratory environments. Assignments such as case studies and group projects that involve the use of apps allow students to gain greater familiarity with the capabilities of mobile technology. This integrated approach promotes facility and proficiency with smartphones and may enhance consistency and accuracy when used in clinical settings. The use of mobile apps may also aid students in becoming more responsible in their use of smartphones as a resource (George & DeCristofaro, 2016). A study entitled “Smartphone Application for Educating Undergraduate Nursing Students about Care for Infant Airway Obstruction” was conducted in Korea. The study posited that smartphone-based education may be an effective method to utilize in nursing education related to teaching airway obstructions in infants (Kim et al., 2017). Another study was conducted with the aim of investigating the effect of software facilitated teaching on final grades of dental students in a dental morphology course in Saudi Arabia. The findings revealed that students who utilized this technology performed substantially better in final examinations than those who did not. The addition of computer-based learning methods was found to enhance students’ learning and educational outcomes (Al-Thobity et al., 2017).
In 2021, Radmard and his colleagues conducted a study titled “The effect of smartphone ventilator training application (VT App) on the knowledge and skills of intensive care unit nurses”. The findings revealed that nurses who utilized the application gained increased knowledge and skills in the ICU. This proved that smartphone-based training programs have the potential to improve the proficiency of nurses in the intensive care setting.
A research study was conducted in Korea to investigate the effects of an interactive nursing skills mobile application on nursing students’ knowledge, self-efficacy, and skills performance. The results demonstrated the effectiveness of this learner-centered mobile application for practical nursing skills education. Developing and implementing a mobile application with a wide spectrum of nursing content specifically designed to engage students across a spectrum of nursing fields of study is recommended. This approach would promote greater overall skill proficiency in students(Kim & Suh, 2018).
Recent studies have revealed the positive impact of smartphone-based technologies on nursing education. Several applications for ventilator training are currently available and can be easily downloaded and used on smartphones. However, the available content within these applications has been found to be outdated and lacking in depth, making them insufficient for nurses’ training needs. Furthermore, few research studies have been conducted on training nurses on ventilators and mechanical ventilation using smartphone applications. This highlights the need to develop and test new smartphone-based training programs for ventilators and mechanical ventilation (Radmard et al., 2021). Therefore, this study was conducted with the aim of investigating the effect of a competency-based educational application on the knowledge and skills of working with a ventilator in nursing students.
Methods
Study Design and Sample
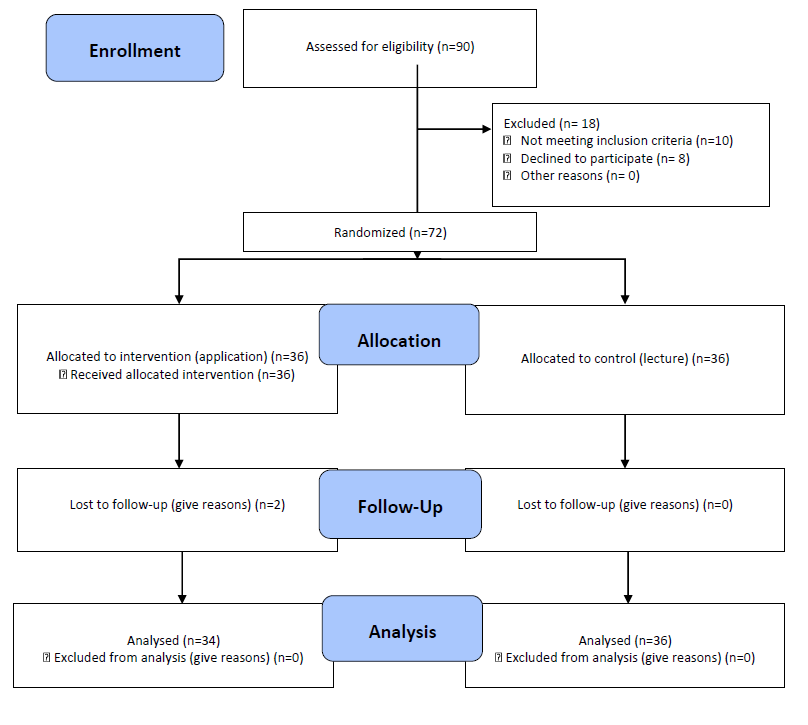
This study used a randomized clinical trial with a pre-test-post-test design and a control group. The research population in this study was fourth semester nursing undergraduate students. By obtaining permission from the educational vice-chancellor of Shahid Sadoqi Nursing School of Yazd and receiving the list of the names of the fourth semester undergraduate nursing students for sampling, these students were selected in purposeful sampling using simple randomization and lottery to divide them into two groups: a control and an intervention group.One important consideration is that the nursing school had previously divided fourth-semester students into two groups (at the beginning of the academic year): a first group of non-native students and a second group of native students. The first group was used as the control for the lecture-based classroom teaching, while the second group was trained using the competency-based mobile application. The aim of this separation was to prevent the transfer of information between groups. The number of undergraduate nursing students studying in the fourth semester in groups one (control) and two (intervention) was a total of 45 people in each class, and finally, according to the inclusion criteria and the lack of exclusion criteria, 36 people were considered for each group. From each class and among the eligible students who were willing to participate in this research, a total of 72 students participated in the study.
Setting and Sample Criteria
Students entered the study after completing an informed consent form. The sample size was based on the results of a similar study by Keegan, which used a screen-based computer simulation in the field using a virtual ventilator to teach the principles of mechanical ventilation (Keegan et al., 2009), taking into account the confidence factor of 95% (equal to 1.96) and the test power of 90% (equal to 1.31), 32 people were obtained for each group. Considering the probability of a 10% sample dropout, 36 students were selected for each group. The criteria for entering the study included studying in the second year and fourth semester of the Bachelor of Nursing program, and students’ willingness to participate. In the study, the inclusion criteria required participation in all educational stages of the study, participation in the practical training session to work with a ventilator, having a mobile phone equipped with the Android operating system, and the exclusion criteria included participation in similar educational programs, experience in working with a ventilator, or students on study or sick leave.
Two people from the intervention group did not continue the training process with the application and were excluded from the study, thus a total of 70 people remained and were included in the final statistical analysis. The data related to the knowledge of working with a ventilator before and after the intervention, as well as the data related to the skill of working with a ventilator after the intervention were measured and compared. This clinical trial study, with the aim of standardizing the results report, used the CONSORT statement, which is a manual that includes the stages of design, implementation and results reporting (Figure 1). Nursing students of the fourth semester of the Bachelor of Nursing program participated in the study during the period from September 23, 2023, to November 8, 2023.
Figure 1
CONSORT Flow Diagram
Instruments and Data Collection
The data collection tools used in this study included a demographic information questionnaire, ventilator knowledge assessment questionnaire and ventilator skill assessment form using an Objective Structured Clinical Examination (OSCE) test and a checklist for recording the time and correctness of ventilator settings. The data collection in this study was self-reporting; in this way the questionnaire was provided to the students at the right time, and they were asked to answer the questions with focus and accuracy.
Students in both the control and intervention groups were asked to complete the demographic information form (including age, sex, the grade point average (GPA) from the previous semester) and the knowledge assessment questionnaire about working with ventilators (pre-test).
Knowledge assessment questionnaire
The knowledge assessment questionnaire was created by the researcher and was designed as 20 multiple-choice questions on selected topics related to ventilators based on books and reliable sources, and each correct answer was given one mark. The questions included knowing the selected modes of the ventilator, the location of the parameters, and how to change the parameters, which were matched with the criteria for setting multiple-choice questions (question design criteria and rules).
To measure face and content validity, the designed questionnaire was provided to five faculty members of the nursing department and five nurses with master’s degrees in special care nursing working in the special care department. After feedback, the desired corrections were made. After verifying the face and content validity, the questionnaire was designed electronically and was given to 44 eighth semester nursing students and they were asked to answer the questions. Then they were asked again two weeks later to answer the questionnaire. The reliability index calculated by Cronbach’s alpha in this method was reported as 0.872, which is acceptable. The final questionnaire had 20 questions. Each correct answer was given one point. The range of questionnaire scores varied from 0 to 20. Getting more marks meant more knowledge was evident.
After the implementation of the pre-test, the training process began, and first, the training software was installed in the cell phones of the students of the intervention group in a one-hour session, and the students were taught how to use it, and it was made available to the students for a month. After a period of 30 days the training process with the training application was completed.
After 30 days of the study’s duration, the control group received the lecture-based conventional education, during which the instructor presented a lecture with the aid of educational slides at the College of Nursing and Midwifery. Ten days after holding the lecture training session, the knowledge survey questionnaire in the field of working with ventilators (post-test) was completed. At the end of the training time with the competency-based educational application to work with a ventilator, on the 30th day of study, the researcher’s user panel, which contained the information of all students, was checked and the names of those who had completed the training process were identified and recorded; Then, for the students who passed all the steps and passed the final exam with the control group received the lecture-based conventional education, on the 40th day (simultaneously with the post-test), two hours of practical training was held on the real ventilator without the presence of a patient.
Then all the students practiced for an hour and if they had any problems, they asked the teacher their questions. Then, the OSCE ventilator skill test with a checklist to record the time and correctness of the ventilator settings was held seven days after this practical training session, and the time required to make the ventilator settings, and the scores related to the correctness of the ventilator settings in both groups of training with the application. Competency based on the ability to work with a ventilator and the lecture group was measured using the OSCE test. Higher scores and shorter duration indicated greater skill in working with the ventilator.
OSCE test
The OSCE test consisted of five stations. These five stations were as follows: the first station was to turn on the device and perform basic settings based on the gender, height and weight of the hypothetical patient with five items, the second station was to set the volume controlled CMV mode with six items, the third station was to set the SIMV mode with nine items in the station. The fourth station was focused on SPONT mode adjustment with five items, and the fifth station included PSV pressure support mode adjustment with five items: in all, there was a total of 30 items.
A checklist was designed and used to measure and record the score and time of each section and settings parameters. Items related to setting the ventilator and modes in this OSCE test were selected based on the setting of the most used modes in the special care department where the scenario was developed. Each test station was assessed and approved by 10 experts.
The study evaluators were taught how to score according to the relevant checklist. The skill of working with the ventilator was evaluated by a researcher-made checklist. The time spent performing each scenario was also recorded for each participant with a stopwatch. Higher scores and shorter duration indicated greater skill in working with the ventilator.
To determine the face and content validity, scenarios and checklists were provided to five faculty members and five nurses working in the intensive care unit, so that if they have an opinion about it, they could reflect it to the research team. Then, the requested corrections were applied to the final checklist. To check the reliability of the checklist, ten eighth semester nursing students were asked to participate in the practical evaluation. Each student was asked to adjust the ventilator according to the scenario. A video was made from the content of the student’s activity. The videos were given to the evaluator to give a grade. After ten days, the videos were given to the evaluator again. The reliability of the questionnaire was estimated at 0.930 through retesting, which was acceptable.
Competency-based educational Application
To develop the educational software, web programmers and graphic designers created the interface, including backgrounds and icons. The software, designed for Android smartphones, guides users through eight step-by-step lessons on operating a ventilator. The final step is dedicated to an exam, featuring written content embedded in educational videos. These short video segments aim to help students become more familiar with the real-world ventilator environment.
The software was organized into eight training stages followed by a final test. Progression through the stages was conditional: learners must demonstrate sufficient understanding of each stage before moving on to the next. At the end of each stage, learners completed a set of four multiple-choice quizzes, each containing five questions. To advance, they must score at least 60%. If they did not meet this threshold, they were required to review the content and retake the test after 72 hours. If a learner failed to achieve the required score every 72 hours over a 14-day period, they were moved back one stage (except in the case of the first stage). This approach ensured mastery of the material before progressing to more advanced content.
The restriction on accessing the next stage and the ability to repeat a stage multiple times encouraged learners to study more carefully and retain the material more effectively. After completing all eight stages, students took a final exam. Upon passing, they advanced to the final phase of the application, where they could practice their skills using a ventilator simulator app. This simulator replicated the C2 ventilator model and was developed by the corresponding manufacturer.
In the final section, students entered their email addresses so a valid certificate—issued by the nursing school—could be sent to them. To uphold ethical standards, this competency-based educational application was also made available to students in the lecture-based training group.
The educational software was developed in collaboration with two information technology experts for the Android platform. It was programmed using B4A, which was ultimately converted into Java, and utilized a MySQL database. The user panel was designed using PHP and a Materialize CSS framework. The application supports online access for downloading educational videos and includes a user panel that allows students to submit their information directly to the study researcher. The course is structured into eight stages, with a minimum 72-hour interval between stages (except for the first). As a result, completing the full course requires at least 21 days.
The software features educational video content, written texts, and images, all organized for quick access. Users can view course-related events—such as exam dates and the start and end of each section—through an integrated educational calendar that syncs with the mobile device’s internal calendar. The interface is optimized for both smartphones and tablets.
Practical system features include notifications confirming the completion of each stage or alerts indicating failure to meet the minimum passing score, along with instructions to review the material and retake the exam after 72 hours. At the end of the program, successful completion of the training course was clearly displayed.
To prevent the transfer of education between groups, the application allowed access only to those students who were registered and confirmed by the researcher. Each user had to register their first and last names, contact number, and password to gain access. They were also instructed to not share any of the educational content or personal details with any other users. The educational videos employed in this study were created and edited by the research team. The distribution of educational information was banned to avoid any leaks to the control group or other participants.
To ensure the educational content in the proposed software was appropriate for undergraduate nursing students, input was gathered from a panel of eight experts: three academic supervisors, three nursing graduates with ICU experience, and two faculty members. The content focused on five key areas: (1) principles and types of mechanical ventilation, (2) ventilator parameters and settings, (3) ventilator modes, (4) ventilator alarms, and (5) ventilator adjustments for patients with various medical conditions, including ventilator calibration.
Relevant nursing textbooks in intensive care and medical-surgical nursing were consulted during content development. The draft materials were then reviewed by the expert panel to ensure alignment with the Hamilton C2 ventilator model, and necessary revisions were made. The finalized content was incorporated into the software in both written format and as video recordings from the ventilator simulator environment, making it accessible and engaging for learners.
A user guide was provided to ensure that all authorized users could easily access the software and navigate the educational content. The software is compatible with Android operating systems version 5 and above.
It is important to note that both the application-based and lecture-based groups received identical educational content. This included the same theoretical material, practical training, knowledge and skills assessments, and instructors. The only difference between the two groups was the method of instruction.
QUIS-Questionnaire of User Interface Satisfaction
As a secondary objective of the study, students’ satisfaction with the competency-based educational application for ventilator training was assessed using a standardized questionnaire designed to evaluate usability and user satisfaction. The questionnaire measured satisfaction across five categories: screen design, technology and system information, learning experience, system capabilities, and overall impressions of the software. Each section included multiple questions, with responses rated on a 9-point scale. Scores of 1–2 were considered poor, 3–5 average, 6–8 good, and 9 excellent.
This questionnaire has been used in previous research, and its validity has been established. Its reliability has been confirmed with a reported Cronbach’s alpha coefficient of 0.76 (Hasannejad, 2013; Zerehsaz et al., 2006).
Ethical considerations
To ensure adherence to research ethics standards, students were fully informed about the objectives of the study. The purpose of the research was explained in detail, and written informed consent was obtained from each participant. Students were assured of their right to participate voluntarily and their freedom to withdraw from the study at any time without penalty. Confidentiality of all collected data was strictly maintained by the researchers.
This study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences in Yazd, under the ethics code IR.SSU.REC.1401.091. The ethics approval was granted on February 8, 2023.
Data Analysis
Data analysis began by assessing the normality of the data distribution using the Kolmogorov-Smirnov test. Based on the results, further analysis was conducted using SPSS version 22. Descriptive statistics, including mean and standard deviation, were used alongside inferential statistical tests such as independent and paired t-tests, as well as the chi-square test. The significance level of p < 0.05 was considered statistically significant.
Results
70 eligible students participated in the study, of whom 27 (38.57%) were male and 43 (61.43%) were female. The average age of the students was 20.29 ± 1.28 years, ranging from 19 to 28 years. The average GPA across both groups was 16.37.
An independent t-test showed no statistically significant difference between the two groups in terms of age and GPA (p > 0.05). Similarly, the chi-square test indicated no significant difference in gender distribution between the groups (p = 0.575).
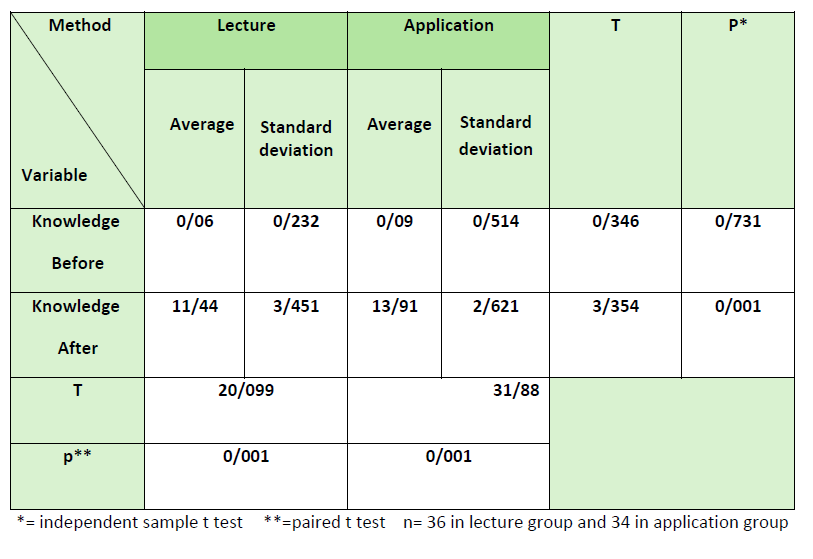
The paired t-test results showed that both training methods significantly improved students’ knowledge scores (p = 0.001). The independent t-test indicated no significant difference between the two groups before training (p = 0.731). However, after training, the group (intervention) using the software scored significantly higher in knowledge level than the lecture (control) group (p = 0.001) (see Table 1).
Table 1
Comparison of the Average Knowledge Scores Between the Two Study Groups Before and One Month After the Intervention
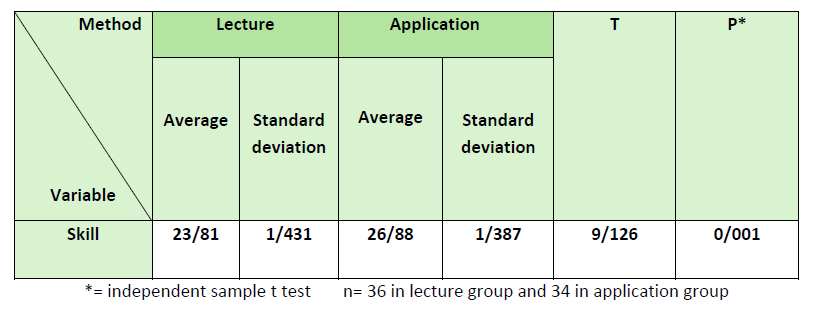
The results of the independent t-test showed that the average ventilator skill score in the software training (intervention) group was significantly higher than in the lecture (control) group (p = 0.001) (see Table 2).
Table 2
Comparison of the Average Ventilator Skill Scores Between the Two Study Groups After the Intervention
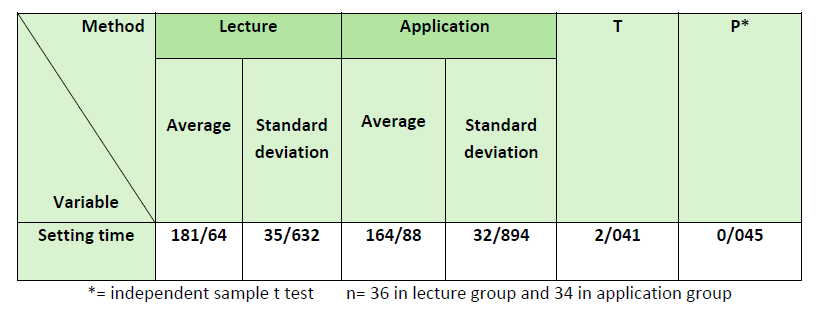
The results of the independent t-test showed that the average time required to set up the ventilator was significantly shorter in the software training (intervention) group compared to the lecture (control) group (p = 0.001) (see Table 3).
Table 3
Comparison of the average ventilator setting time in the two study groups after the intervention
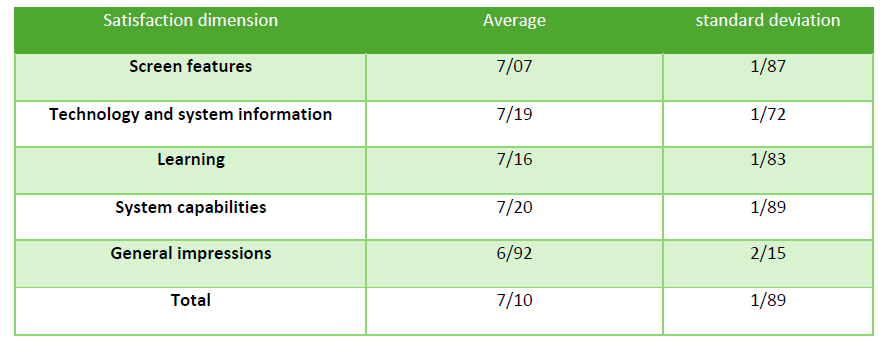
The results of the statistical analysis, including the mean and standard deviation across various dimensions of student satisfaction, indicate that students’ overall satisfaction with the competency-based ventilator training software was at a good level, with an average score of 7.10 (see Table 4).
Table 4
Analysis of Student Satisfaction Dimensions Regarding the Competency-Based Educational Application for Ventilator Training
Discussion
This study aimed to evaluate the effect of a competency-based educational application on nursing students’ knowledge and skills in operating a ventilator. The findings confirmed that the two study groups were comparable in terms of demographic characteristics. The results demonstrated that the use of the competency-based educational application significantly improved students’ knowledge and skills in ventilator operation compared to the traditional classroom lecture method. Thus, the application-based teaching approach effectively enhanced students’ competence in this area.
Additionally, as a secondary objective, the study assessed student satisfaction with the application-based training. The analysis of satisfaction dimensions revealed that students rated this educational method at a good level, indicating a positive learning experience.
The competency of critical care nurses responsible for managing patients on mechanical ventilation is critically important. Continuous development of their knowledge, skills, and capabilities is essential. Educators, nursing students, and practicing nurses should prioritize acquiring and maintaining a comprehensive understanding of mechanical ventilation. This includes knowledge of ventilator mechanics, effective management strategies, and thorough patient assessment techniques, all of which are vital for ensuring optimal patient outcomes (Jun et al., 2016).
According to a study conducted in Iran, senior nursing students demonstrated significant deficiencies in ventilator management skills compared to other clinical competencies. The students reported a low level of competency in operating ventilators and expressed an urgent need to address this skills gap (Azizzadeh Forouzi et al., 2018).
The current deficiency of information about working with ventilators is not restricted to the Iranian healthcare sector, as it is a common concern among ICU nurses in other countries as well. This implies that there is a pervasive lack of knowledge and skill amongst ICU nurses in the global context, and interventions are needed in order to remediate this situation (Radmard et al., 2021).
A study conducted in Australia found that approximately 63% of ICU nurses had not received any formal training in ventilator use prior to working in intensive care units. Additionally, many nurses reported limited familiarity with invasive ventilation, a critical aspect of ventilator management. These findings highlight a global concern: nurses often begin their careers lacking essential knowledge and skills related to mechanical ventilation (Guilhermino et al., 2018; Guilhermino et al., 2014).
Ventilator management is often complex and challenging for trainees, yet its proper application is critical for improving patient outcomes. Therefore, comprehensive education in this area is essential. Nurses must develop a thorough understanding of ventilator modes, their functions and limitations, the causes of respiratory distress, and ventilator-patient dyssynchrony. Equally important is knowing how to effectively manage these issues to deliver high-quality, patient-centered care. Early identification of problems and timely intervention by nurses can help resolve acute respiratory distress, dyspnea, and increased work of breathing, thereby preventing adverse events (Grossbach et al., 2011).
A study by Azizzadeh Forouzi et al. (2018) demonstrated that nursing students readily use smartphones for training purposes in clinical settings. Smartphones have become indispensable devices widely used by nursing students, offering significant potential to enhance both their clinical work and educational experiences. Due to their small size, portability, and easy accessibility, smartphones are now an integral part of daily life. They have transformed human interactions by enabling quick communication and feedback, as well as providing instant access to information, and facilitating data saving, storage, and sharing (Gutiérrez-Puertas et al., 2021).
Smartphones are one of the most popular and influential technologies, fundamentally transforming communication and shaping consumer behavior and attitudes. A large proportion of nursing undergraduate students own smartphones, using them extensively for communication and accessing information. These devices have become essential tools for students, increasingly integrated into their studies for research and educational activities. This trend highlights the growing dependence of the younger generation on smartphones for information and communication (Alsayed et al., 2020).
Smartphones offer significant benefits to nursing students in clinical settings. They assist with tasks such as calculating drug dosages and provide quick access to important health information and clinical resources. These advantages have the potential to improve decision-making and enhance the quality of patient care. However, concerns remain regarding the credibility and reliability of some resources accessed via smartphones. Additionally, smartphones facilitate communication between nursing students and practitioners, enabling the exchange of information, experiences, and advice—an essential aspect of clinical training. This interaction boosts students’ self-efficacy, clinical competence, and efficiency, while also reducing anxiety during clinical practice (Gutiérrez-Puertas et al., 2021).
Despite the large number of healthcare applications available globally, specialized nursing apps, especially those in Persian, have not received adequate attention in Iran. Most existing applications focus on drug selection and dosage calculations, while few addresses critical areas such as ventilator management. This gap is particularly concerning given the growing demand for ventilator-related care (Radmard et al., 2021).
Consistent with these findings, the current study showed a significant increase in nurses’ overall knowledge and skills after the intervention. Several other studies have also explored the use of mobile phones in nursing education, highlighting their potential benefits.
A study conducted in South Korea titled Effects of Rescuers’ Using a Smartphone-Band on the Quality of Chest Compression during Cardiopulmonary Resuscitation—Measured Using a Manikin found that training in basic life support through smartphone software significantly improved knowledge acquisition compared to traditional methods. The researchers concluded that the smartphone-based training was more effective than conventional lectures, resulting in better learning outcomes (Baek & Park, 2015).
Another study conducted in Iran in 2021, titled The Effect of the Smartphone Ventilator Training Application on the Knowledge and Skills of Nurses in Intensive Care Units, found that using smartphone-based ventilator training software significantly improved the knowledge and skills of ICU nurses (Radmard et al., 2021).
A study conducted in the United States titled Using an Educational Mobile Application to Teach Students to Take Vital Signs found that the “Clinic Vitals” mobile application was an effective alternative to in-person instruction. The researchers highlighted that modern educational tools, such as online videos, simulations, and mobile applications can serve as effective teaching methods for nursing education. The study emphasized the potential for further exploration of mobile applications like “Clinic Vitals” to support and enhance nursing education (Hester et al., 2021).
Another study conducted in Shandong, China, investigated the effectiveness of a game-based mobile application for educating nursing students on flushing and locking venous catheters with pre-filled saline syringes through a randomized controlled trial. The results showed that the application significantly improved students’ skills in this procedure. The researchers concluded that the game-based mobile application serves as an effective complement to traditional training methods (Gu et al., 2022).
A study conducted in Iran in 2021, titled “The Effect of Smartphone Application-Based Learning on Intensive Care Nurses’ Knowledge Relating to Arterial Gas Interpretation,” demonstrated the positive impact of using smartphone applications on nurses’ knowledge. The findings suggest that application-based learning can serve as an effective alternative or supplemental tool for teaching essential skills—such as arterial blood gas interpretation—in nursing education (AliKarami, et al., 2021).
In contrast, a study titled “A Smartphone Application to Educate Undergraduate Nursing Students About Providing Care for Infant Airway Obstruction” found that, although the test group showed greater improvement in knowledge compared to the control group, the difference was not statistically significant (Kim et al., 2017).
The discrepancy between the findings of our study and those of Shin Jung Kim et al. (2017) may be attributed to differences in the instructional design and implementation of the educational interventions. In our study, the ventilator training application was competency-based, allowing students in the intervention group unrestricted access to educational content. This design enabled learners to thoroughly engage with the material at their own pace, which likely contributed to the significant improvement observed in their knowledge and skills.
In contrast, the study by Kim et al. (2017) provided mobile-based training content to both the intervention and control groups without clear differentiation or restrictions. As a result, exposure to similar content across groups may have diluted the effects of the intervention. This lack of control over educational exposure could have influenced both groups’ knowledge and self-efficacy, thereby explaining the absence of a statistically significant difference between them.
The difference in the average scores of skills and self-confidence in performance between groups was statistically significant. Therefore, the experimental group showed better skill and self-confidence than the control group. The average total satisfaction score in the test group was higher compared to the control group, but no statistically significant difference was observed between the two groups (Kim et al., 2017).
The inconsistency in findings may also stem from differences in the learner experience and instructional expectations. In the Kim et al., (2017) study, students were likely expected to passively replicate observed procedures, which could have contributed to lower satisfaction levels. Furthermore, participants in the simulation group may have experienced heightened anxiety when engaging with both the simulation and mobile-based content, potentially impacting their learning outcomes and satisfaction.
In contrast, this current study employed a more interactive, engaging, and competency-based design. The application content was structured to actively involve learners, promote self-paced study, and provide feedback, all of which are known to enhance user engagement and satisfaction. This learner-centered approach may explain the higher satisfaction scores observed among students in this study’s intervention group.
A study conducted in 2021 titled “Evaluating the Utilization of a Smartphone Application for Teaching Eye Screenings to Opticians” found that the TEACHES-LEM application was as effective as face-to-face training (F2FT) in educating opticians (Chee et al., 2021). The differences in outcomes between this study and our research may be attributed to the distinct characteristics of the educational applications used in each.
The application implemented in our study offered several advanced features—such as segmented educational texts and videos, modular content delivery, unrestricted access regardless of time or place, and a competency-based progression system requiring students to achieve a specific level of knowledge to advance and ultimately complete the training. These interactive and learner-centered elements likely contributed to higher knowledge retention, engagement, and satisfaction, distinguishing our application from the one utilized in Chee et al.’s (2021) study.
A study on nursing education and student satisfaction with the use of an emerging mobile learning tool revealed mixed outcomes. According to the findings, 32.4% of students found the educational content to be very useful, while 14.7% reported partial satisfaction. Notably, 52.9% indicated difficulty in utilizing the resource effectively. These results suggest that, despite the potential of mobile learning tools, challenges remain regarding the quality of educational content, curriculum integration, and the usability of such technologies. The study recommended improvements in both the instructional design and the accessibility of mobile learning tools to enhance their effectiveness in nursing education (Maag, 2006).
In summary, the findings of this study demonstrated that nursing students in the training group who used the competency-based educational application for ventilator management achieved significantly higher knowledge scores, demonstrated greater proficiency and speed in ventilator settings, and exhibited enhanced practical skills compared to those in the lecture-based group. Furthermore, student satisfaction with the educational application—evaluated as a secondary outcome—was reported to be at a good level. These results support the recommendation that competency-based educational applications be integrated into nursing curricula as an effective strategy to enhance students’ knowledge and practical skills in ventilator management.
Conclusion
Students in the training group who used the competency-based educational application for ventilator management demonstrated significantly higher knowledge scores, greater proficiency in ventilator settings, and faster response times compared to those in the lecture-based group. Additionally, the level of satisfaction with the educational application which was evaluated as a secondary outcome, was reported to be at a good level. Based on these findings, the use of a competency-based educational application is recommended as an effective strategy to enhance the knowledge and practical skills of nursing students in ventilator management.
Author Bios
Hadis Ghasemimilsefid
MSc in Intensive Care Nursing, Research Centre for Nursing and Midwifery Care,Non-communicable Diseases Research Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Mostafa Javadi
PhD in Nursing, associate Professor, Research Centre for Nursing and Midwifery Care, Non-communicable Diseases Research Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Khadijeh Nasiriani
PhD in Nursing, Professor, Research Centre for Nursing and Midwifery Care,Non- communicable Diseases Research Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Acknowledgements
We extend our sincere gratitude to the students who contributed to this study. We are also grateful to the Shahid Sadoughi University of Medical Sciences and Health Services, as well as all the study participants, for their invaluable support and participation.
References
Al-Thobity, A. M., Farooq, I., & Khan, S. Q. (2017). Effect of software facilitated teaching on final grades of dental students in a dental morphology course. Saudi Medical Journal, 38(2), 192. doi: 10.15537/smj.2017.2.15627
AliKarami, F., Rejeh, N., Heravi K., Majideh, T., Seyed D., & Parvaresh M. M. (2021). The effect of smartphone application-based learning on intensive care nurses’ knowledge about the arterial gas interpretation. Iranian Journal of Nursing Research, 16(2), 49-58.
Alsayed, S., Bano, N., & Alnajjar, H. (2020). Evaluating practice of smartphone use among university students in undergraduate nursing education. Health Professions Education, 6(2), 238-246. doi: 10.1016/J.HPE.2019.06.004
Azizzadeh Forouzi, M., Alimirzaei, R., Dehghan, M. & Heidarzadeh, A. (2018). Evaluation of nursing students’clinical skills in intensive care units. Journal of Nursing Education, 6(6). doi:10.21859/jne-06068
Baek, H. S. & Park, S. S. (2015). Effects of rescuers’ using a smartphone-band on the quality of chest compression during cardiopulmonary resuscitation-measured using a manikin. Indian Journal of Science and Technology, 8(18), 1. doi: 10.17485/ijst/2015/v8i18/75912
Chee, W.K., Yip, C.C., Yang, L., Soo, Y.K., Wang, J., & Chang, B.C.M. (2021). Assessing the use of a smartphone app to teach eye screening to opticians. The Clinical Teacher, 18(3), 258-263. doi: 10.1111/tct.13310
Clemons, J., & Kearns, M. (2016). Invasive mechanical ventilation. Hospital Medicine Clinics, 5(1), 17-29. doi: 10.1016/j.ehmc.2015.08.003
George, T. P, & DeCristofaro, C. (2016). Use of smartphones with undergraduate nursing students. Journal of Nursing Education, 55(7), 411-415. doi: 10.3928/01484834-20160615-11
Grossbach, I., Chlan, L., & Tracy, M. F. (2011). Overview of mechanical ventilatory support and management of patient-and ventilator-related responses. Critical Care Nurse, 31(3), 30-44.
Gu, R., Wang, J., Zhang, Y., Li, Q., Wang, S., Sun, T., & Wei, L. (2022). Effectiveness of a game-based mobile application in educating nursing students on flushing and locking venous catheters with pre-filled saline syringes: A randomized controlled trial. Nurse Education in Practice, 58, 103260. doi: 10.1016/j.nepr.2021.103260
Guilhermino, M. C., Inder, K. J., & Sundin, D. (2018). Education on invasive mechanical ventilation involving intensive care nurses: A systematic review. Nursing in Critical Care, 23(5), 245-255. doi: 10.1111/nicc.12346
Guilhermino, M. C., Inder, K. J., Sundin, D., & Kuzmiuk, L. (2014). Education of ICU nurses regarding invasive mechanical ventilation: Findings from a cross-sectional survey. Australian Critical Care, 27(3), 126-132. doi: 10.1016/j.aucc.2013.10.064
Gutiérrez-Puertas, V., Gutiérrez-Puertas, L., Aguilera-Manrique, G., Rodríguez-García, M. C., & Márquez-Hernández, V. V. (2021). Nursing students’ perceptions of smartphone use in the clinical care and safety of hospitalised patients. International Journal of Environmental Research and Public Health, 18(3), 1307. https://doi.org/10.3390/ijerph18031307
Hasannejad, M. (2013). Developing a web-based system for self-care management of type 1-diabetes [dissertation]. Tehran: Iran University of Medical Sciences.
Hester, L., Reed, B., Bohannan, W., Box, M., Wells, M., & O’Neal, B. (2021). Using an educational mobile application to teach students to take vital signs. Nurse Education Today, 107, 105154. doi: 10.1016/j.nedt.2021.105154
Jun, J., Kovner, C. T, & Stimpfel, A. W. (2016). Barriers and facilitators of nurses’ use of clinical practice guidelines: An integrative review. InternationalJournal of Nursing Studies, 60, 54-68. doi: 0.1016/j.ijnurstu.2016.03.006
Keegan, R., Henderson, T., & Brown, G. (2009). Use of the virtual ventilator, a screen-based computer simulation, to teach the principles of mechanical ventilation. Journal of Veterinary Medical Education, 36(4), 436-443.
Kim, H., & Suh, E. E. (2018). The effects of an interactive nursing skills mobile application on nursing students’ knowledge, self-efficacy, and skills performance: A randomized controlled trial. Asian Nursing Research, 12(1), 17-25. doi: 10.1016/j.anr.2018.01.001
Kim, S. J, Shin, H., Lee, J., Kang, S., & Bartlett, R. (2017). A smartphone application to educate undergraduate nursing students about providing care for infant airway obstruction. Nurse Education Today, 48, 145-152. doi: 10.1016/j.nedt.2016.10.006
Maag, M.. (2006). Ipod, upod? An emerging mobile learning tool in nursing education and students’ satisfaction. Paper presented at the Who’s learning? Whose technology? Proceedings ASCILITE 2006.
Mohamed, A. B., Abdel-Aziz, M. A., Mehany, M. M., & Morsy, K. M.. (2019). Effect of educational program on nurses’ knowledge and practice caring for patients on mechanical ventilation. Assiut Scientific Nursing Journal, 7(19), 131-141. doi:10.21608/asnj.2019.74126
Phillippi, Julia C, & Wyatt, Tami H. (2011). Smartphones in nursing education. CIN: Computers, Informatics, Nursing, 29(8), 449-454.
Radmard, M. H., Alavi, N. M., & Sadat, Z. (2021). The effect of smartphone ventilator training application on the knowledge and skills of intensive care unit nurses. International Archives of Health Sciences, 8(4), 225-230. doi: 10.4103/iahs.iahs_107_21
Reynolds, A., Osborne, T. F., Waggoner, J., Melton, R., Motarjemi, R., Schulze, J. P, & Chau, D. (2018). Advances in health education technology. In D. Chau & . F. Osborne. (Eds.) Using Technology to Improve Care of Older Adults, (pp. 287-306), Springer. doi: 10.1891/9780826142436
Urner, M., Ferreyro, B. L., Douflé, G., & Mehta, S. (2018). Supportive care of patients on mechanical ventilation. Respiratory Care, 63(12), 1567-1574. https://doi.org/10.4187/respcare.06651
Windisch, W., Geiseler, J., Simon, K., Walterspacher, S., Dreher, M., & on behalf of the Commission Guideline. (2018). German national guideline for treating chronic respiratory failure with invasive and non-invasive ventilation: Revised edition 2017–part 1. Respiration, 96(1), 66-97. https://doi.org/10.1159/000488667
Wyatt, T, & Krauskopf, P. (2012). E-health and nursing: Using smartphones to enhance nursing practice. Online Journal of Nursing Informatics (OJNI), 16(2), 1706
.Zerehsaz, M, Fattahi, R, & Davarpanah, M. (2006). Investigation and analysis of elements and features discussed in the Simorgh user interface software and determine students’ satisfaction from interacting with this user interface. Library and Information Science, 9(4), 127-150.